Platelet Rich Plasma: PRP for Dry Eyes
Platelet-rich plasma (PRP) is a common treatment nowadays in the cosmetic dermatological field. It stimulates fibroblasts within the skin and makes them produce collagen fibers. As PRP is made from one’s self blood, the treatment is regarded as very safe. The problem exists in rather a high cost of the PRP processing kit. New research shows PRP may help with Dry Eyes.
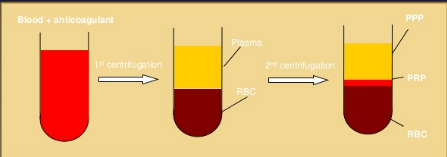
The difference between PRP and Autologous Serum is that PRP uses a solution which breaks up the cellular membranes of the platlets which are thought to have extra growth factors. Platelet-rich plasma (PRP) contains more concentrated platelets than whole blood and can be obtained via centrifugation from whole blood mixed with anticoagulant. Platelets are critically important in the wound-healing process.
Autologous Serum is made by drawing a patient’s blood and then extracting the serum via centrifuge. The serum is mixed with artificial tears to create several autologous tear vials. Typically, a patient receives eight to 12 vials, which can be frozen and stored until required. Studies have shown that freezing the drops effectively preserves the stability of essential autologous components, including epidermal growth factor, vitamin A and transforming growth factor beta. Also, no bacterial contamination has been documented in vials that were stored properly. I have never seen an ulcer from Autologous Serum, but it is imperative that the patients follows the instructions properly: to never leave them un-refrigerated as they have no preservative or other anti-bacterial element other than its inherent properties. Autologous Serum similarly has growth and healing factors but PRP is thought to have a higher concentration.
A newer term has now been used for PRP:
Plasma rich in growth factors (PRGF) eye drops consists on a platelet-enriched plasma in which platelets have been degranulated to release all stored growth factors. The resulting eye-drops, once filtered, is rich in biologically active mediators such as growth factors, neurotrophic agents, vitamin A and fibronectin and does not contain high levels of pro-inflammatory molecules (Anitua et al., 2011)
We have used Autologous Serum for years at Visionary Eye Doctors. I have used Autologous Serum for over 15 years at Harvard Medical School and now at Visionary. I have never seen a complication from using one’s own Serum. I can still count on 1 hand the number of patients who have not benefited from AS. In the rare patient who does not benefit from AS, we will now start to offer Platelet Rich Plasma.
Sandra Lora Cremers, MD, FACS
References:
Acta Ophthalmol. 2015 Dec;93(8):e605-14. doi: 10.1111/aos.12710. Epub 2015 Apr 2.
Autologous serum and plasma rich in growth factors in ophthalmology: preclinical and clinical studies.
Exp Eye Res. 2016 Oct;151:115-21. doi: 10.1016/j.exer.2016.08.012. Epub 2016 Aug 25.
PRGF exerts more potent proliferative and anti-inflammatory effects than autologous serum on a cell culture inflammatory model.
The mechanism of action of autologous PRP is likely to be the same as that of autologous serum, with the difference being a higher concentration of growth factors, which might stimulate the growth of epithelial cells and thus lead to faster healing. The high concentrations of epitheliotrophic growth factors also have an effect on tightening the epithelial adhesion complex. Alio et al. [26] concluded that autologous PRP promoted healing of dormant corneal ulcers and was accompanied by reduction in pain and inflammation. Hartwig et al. [32] reported a superior effect on cell growth in platelet releasates than in serum owing to its high content of growth factors and concluded platelet releasate could be a novel treatment option for ocular surface defects. We previously reported the effects of autologous PRP on persistent corneal epithelial defect after infectious keratitis. The platelet concentration in PRP prepared in our standardized protocol was approximately 1.5-fold higher than in whole blood, and the PRP also contained significantly higher concentrations of EGF and TGF-β1. We concluded that PRP eye drops are an effective, novel treatment option for chronic ocular surface disease, and that this might be attributable to its high concentration of platelet-contained growth factors [28]. On the basis of this observation, we have started using PRP eye drops in the treatment for patients with RCE.
Ophthalmic Res. 2016 Jul;56(2):68-73. doi: 10.1159/000444496. Epub 2016 May 28.