Fuchs’ Dystrophy
Before you have cataract surgery, be sure you do not have Fuchs’ Dystrophy. This can easily be overlooked even by the best eyeMDs in the world. If you have a family history of Fuchs’, ask your eyeMD to be sure you do not have Fuchs’.
Fuchs’ Dystrophy is an abnormality of the back surface of the cornea that causes the important endothelial cells (which make the cornea clear by pumping out fluid) to malfunction. This can cause the cornea to become cloudy and thus cause significant glare, though vision can still be 20/20 initially. Depending on specifics, your symptoms (in addition to h/o of glaucoma & ERM) are possible. See eyedoc2020@blogspot.com for references on Fuchs
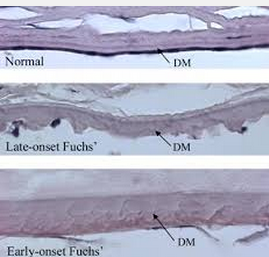
This is what your eyeMD sees on slit lamp, microscopic examination when significant. There is a spectrum of changes that we can see under the microscope and this is advanced.
Pathologically, a cornea from a patient with Fuchs’ dystrophy looks like this above where unusual material or “excrescences” form which seem to push the endothelial cell to the side and make it malfunction and die.
In the end, if the condition worsens, which does NOT happen in every patient necessarily, the cornea will swell and become hazy. Most patients would be more likely to experience this after cataract surgery (where a great deal of energy is used to remove a hard cataract) so we recommend early cataract surgery in patients with Guttae (these areas of abnormal endothelial cells) or Fuchs’ Dystrophy.
Sandra Lora Cremers, MD, FACS
Below: Adapted from: http://www.mayoclinic.org/diseases-conditions/fuchs-dystrophy/basics/definition/con-20023893
Fuchs’ (fooks) dystrophy affects the cornea — the clear front window of your eye. This disorder causes swelling in the cornea that can lead to glare, cloudy vision and eye discomfort.
Fuchs’ dystrophy usually affects both eyes and can cause your vision to gradually worsen over many years. But most people with Fuchs’ dystrophy have a mild type and don’t notice much change in their eyesight.
Some medications and self-care steps may help relieve your Fuchs’ dystrophy signs and symptoms. But when the disorder is advanced and you’ve lost vision, the only way to restore vision is with cornea transplant surgery.
Glare, which is an early symptom and reduces contrast perception or affects vision in low light.
As the disease progresses, Fuchs’ dystrophy symptoms usually affect both eyes and may include:
When your ophthalmologist examines your cornea, he or she looks for:
If you experience some of these signs and symptoms, and especially if they get worse over time, see an eye specialist (ophthalmologist). If symptoms develop suddenly, call an ophthalmologist for an urgent appointment. Other eye conditions that cause the same symptoms as Fuchs’ dystrophy also require prompt treatment.
Normally, the cells lining the inside of the cornea (endothelial cells) help maintain a healthy balance of fluids within the cornea. Healthy endothelial cells prevent the cornea from swelling and help keep the cornea clear. But with Fuchs’ dystrophy, the endothelial cells slowly die off, and probably do not function correctly, resulting in fluid buildup within the cornea (swelling or edema). This causes corneal thickening and blurred vision.
Fuchs’ dystrophy can be inherited. The genetic basis of the disease is complex — family members can be affected to very variable degrees, and sometimes not at all.
Factors that increase your risk of developing Fuchs’ dystrophy include:
- Being female, as Fuchs’ dystrophy is slightly more common in women than in men
- Having a family history of Fuchs’ dystrophy
- Being over 50
- SMOKING can make Fuchs’ worse and worsens prognosis for recovery after treatments (see below reference).
You may undergo tests such as the following so that your doctor can determine whether you have Fuchs’ dystrophy. These tests will also measure the shape, clarity and thickness of the cornea.
- Visual test. You’ll be asked to read letters and numbers on a chart to measure how well you see at various distances. This is called a visual acuity test and is a routine part of eye exams.
- Staging. Your doctor will try to determine the stage of your condition by examining your eye with an optical microscope (slit lamp). He or she will then study the cells lining the back surface of your cornea (endothelial cells). If you have irregular bumps (guttae) on the back surface of the cornea, you may have Fuchs’ dystrophy.
- Corneal pressure test (intraocular pressure or IOP). Your doctor may numb your eyes with drops and then briefly touch your eye with a special instrument that measures eye pressure.
- Corneal thickness (Pachymetry). Your doctor may use a special instrument to measure the thickness of the cornea.
- Corneal Endothelial cell count (ECC): Sometimes your doctor might use another special instrument to record the number, shape and size of the cells that line the back of the cornea.
Some nonsurgical treatments and self-care strategies may help relieve your Fuchs’ dystrophy signs and symptoms. If you have severe disease, your doctor may suggest surgery.
Most people who have surgery for advanced Fuchs’ dystrophy experience much better vision and remain symptom-free for years afterward. Surgical options include:
Clinical trials involve studies of new ways to diagnose or treat a condition. They don’t always offer a definite diagnosis or cure. But they may allow you to benefit from the latest knowledge about Fuchs’ dystrophy. Ask your doctor if you’re eligible for any clinical trials.
In addition to following your doctor’s instructions for care, you can try these techniques to help reduce glare or make your eyes feel better.
References:
Zhang X, Igo RP Jr, Fondran J, Mootha VV, Oliva M, Hammersmith K, Sugar A, Lass JH, Iyengar SK; Fuchs‘ Genetics Multi-Center Study Group.
Invest Ophthalmol Vis Sci. 2013 Aug 27;54(8):5829-35. doi: 10.1167/iovs.13-11918.