Headache and Migraine Diet
Sandra Lora Cremers, MD, FACS
Headaches and Migraines can present in different ways depending on a patient’s particular brain-flow pattern, internal and external conditions (e.g., general medical health, immunological condition, hormones, hydration, humidity). Pain in the head or even seeing bright or dark spots in vision without a headache or flashing lights with or without a headache (assuming vitreous and retinal exam is normal) can be due to an alteration in the blood flow to particular parts of the brain and represent a migraine or Ophthalmic Migraine.
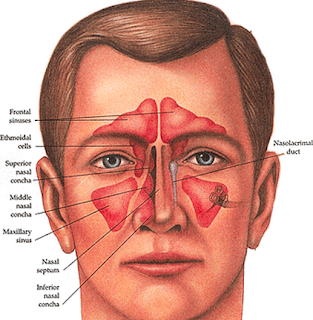
3. Check sinuses: first push on sinus are to see if it uncomfortable/painful: sometimes a CT with contrast or MRI is needed.
4. Request a full neurologic examination
A. Keep headache/migraine diary: when is it really bad; when are your good days & why? Note: visual symptoms, dizziness, light sensitivity and look for any association with:
14. Pregnancy: Check to see if you are pregnant.
15. Note there are many causes of headache. The last two are much rarer but if you ever have the worst headache in your life, you need to call 911 or go to ER as soon as possible. If you have a family history of either of these two, let your MD know if you have any new headache:
Aneurysm
Brain Tumor (benign or malignant)
B. Preventative Remedies: Over the counter:
mg:
(Riboflavin; not just a B vitamin): 400mg/day; Read Reference below prior to taking.
per day. Read Reference below prior to taking.
; Read Reference below prior to taking.
C. If nothing works, some patients try FASTING under Medical Guidance with a well-experienced MD or clinic. There are many kinds of Fasting: It is always best to Fast under the supervision of an MD. If you are Metformin or any of the medications listed below ** only fast UNDER the supervision of an experienced MD.
1. Time restricted Fasting
2. Intermittent Fasting
3. Prolonged Fasting
a. Water Only Fasting for 5-45days under MD supervision
b. Fasting Mimicking Diet (FMD): Dr. Longo developed
Sandra Lora Cremers, MD, FACS
References:
http://www.migrainetrust.org/assets/x/50129
|
Food Type
|
Recommended
|
Not Recommended
|
|
Beverages
|
DRINK AT LEAST 64Oz WATER per day: most common cause of headache & migraines is DEHYDRATION.
Max 6oz/day decaffeinated coffee, Non-citric fruit juices, Max 4oz/day white wine. Herbal teas without citrus, club soda, non-cola soda (ex 7up, ginger ale, etc). Max 2oz/day vodka
White chocolate
|
Red wine, port, coffee, champagne, tea, iced tea, caffeinated sodas
Chocolate or cocoa
|
|
Breads and Cereals
|
Commercial breads: white, whole wheat, rye, French, Italian, English muffins, melba toast, crackers, rye, crisp, bagel
All hot and dry cereals: cream of wheat, wheaten, oatmeal, cornflakes, puffed rice and wheat
|
Avoid the following for sure, but I still recommend avoiding all gluten for at least 3 months and keeping a headache diary to see if this helps each patients:
Hot, fresh homemade yeast breads and crackers with cheese, croutons
Fresh yeast coffeecake, doughnuts, sour dough breads
Any breads containing chocolate or nuts
|
|
Dairy
|
Milk (2% or skim)
Cheese: American, cottage, farmers, ricotta, cream cheese, egg
Yogurt: limit to 4 oz per day
|
Some patients are particularly sensitive to dairy, others are note; there are some theories it may be related to blood type (but I have not seen any good studies to prove this yet);
Cultured dairy such as buttermilk, sour cream, chocolate milk
Cheese: blue, boursoult, brie types, camemberts, cheddar, swiss, gouda, Roquefort, stilton, mozzarella, parmesan, provolone, romano, and emmenlaler
|
|
Desserts
|
Sherberts, ice cream cakes and cookies without chocolate or yeast, Jell-O
|
All sugars increase inflammation so it is a good idea to avoid as much as possible:
Chocolate in ice cream, pudding, cookies, cakes |
|
Sweets
|
Sugar, jelly, jam, honey, hard candy
|
|
|
Food Type
|
Recommended
|
Not Recommended
|
|
Fruits
|
Any fruit juice such as prune, apple, cherry, apricot, peach, pear and fruit cocktail
Limit intake to ½ cup orange, grapefruit, tangerine, pineapple, raspberry, plums, raisins, papaya, passion fruit
|
Avocados, banana ( ½ allowed per day) lemon, lime
All nuts, peanut butter
|
|
Meat, Fish, and Poultry
|
Fresh or frozen turkey, chicken, fish, lamb, veal, pork, tuna
|
Aged, canned, cured, tenderized, processed meats, canned or aged ham, pickled herring, salted dried fish, chicken liver, aged game, hot dogs, sausage, bologna, salami, pepperoni, beef jerky, liver, any meal prepared with marinade
|
|
Sweets
|
Sugar, jelly, jam, honey, hard candy
|
|
|
Miscellaneous
|
Salt in moderation, lemon juice, butter or margarine, cooking oil, whipped cream, and white vinegar. Commercial salad dressings in small amounts as long as they don’t have additives to avoid
|
|
Categories
|
Triggers
|
Examples
|
|
Dietary
|
Skipping meals/fasting
Specific foods
Medications
|
Overuse of over-the-counter medications can cause rebound headaches. Also, missed medication doses and certain medications (e.g. nitroglycerine, indomethacin) may cause headaches.
|
|
Sleep
|
Change in sleep patterns
|
Napping, oversleeping, too little sleep
|
|
Hormonal
|
Estrogen level changes and fluctuations
|
Menstrual cycles, birth control pills, hormone replacement therapies, peri-menopause, menopause, ovulation
|
|
Environmental
|
Weather
Bright Lights
Odors/Pollution
Other
|
Weather and temperature changes, extreme heat or cold, humidity, barometric pressure changes
Bright or glaring lights, fluorescent lighting, flashing lights or screens
Smog, smoke, perfumes, chemical odors
High altitude, airplane travel
|
|
Stress
|
Periods of high stress, including life changes
Accumulated stress
Reacting quickly and easily to stress
Repressed emotions
|
Factors related to stress include anxiety, worry, shock, depression, excitement, mental fatigue, loss and grief.
Both “bad stress” and “good stress” can be trigger (or prevent) migraines. Other triggers can include unrealistic timelines or expectations of oneself.
|
|
Physical
|
Overexertion
Injuries
Visual triggers
Becoming tired or fatigued
|
Over-exercising when out of shape, exercising in heat, marathon running
Eyestrain (if you wear glasses, make sure your prescription is current), bright or glaring lights, fluorescent lighting, flashing lights or computer screens
|
**
If you take the following Medications, do not FAST on your own. Discuss with your MD first and stay under MD supervision.
Metformin
Fenofibrate: (Moderate) Dose reductions and increased frequency of glucose monitoring may be required when antidiabetic agents are administered with fibric acid derivatives (e.g., clofibrate, fenofibric acid, fenofibrate, gemfibrozil). Fibric acid derivatives may enhance the hypoglycemic effects of antidiabetic agents through increased insulin sensitivity and decreased glucagon secretion.
Fenofibric Acid: (Moderate) Dose reductions and increased frequency of glucose monitoring may be required when antidiabetic agents are administered with fibric acid derivatives (e.g., clofibrate, fenofibric acid, fenofibrate, gemfibrozil). Fibric acid derivatives may enhance the hypoglycemic effects of antidiabetic agents through increased insulin sensitivity and decreased glucagon secretion.
Gemfibrozil: (Major) Dose reduction of rosiglitazone may be needed if given with gemfibrozil. Gemfibrozil results in increased rosiglitazone exposure and increases the risk for hypoglycemia. Gemfibrozil is a potent inhibitor of CYP2C8 and rosiglitazone is primarily metabolized via CYP2C8. Concomitant administration of gemfibrozil (600 mg twice daily) and rosiglitazone (4 mg once daily) for 7 days increased rosiglitazone AUC by 127%, compared to the administration of rosiglitazone (4 mg once daily) alone. Fibric acid derivatives also enhance the hypoglycemic effects of antidiabetic agents through increased insulin sensitivity and decreased glucagon secretion.
Lanreotide: (Moderate) Monitor blood glucose levels regularly in patients with diabetes, especially when lanreotide treatment is initiated or when the dose is altered. Adjust treatment with antidiabetic agents as clinically indicated. Lanreotide inhibits the secretion of insulin and glucagon. Patients treated with lanreotide may experience either hypoglycemia or hyperglycemia.
Octreotide: (Moderate) Monitor patients receiving octreotide concomitantly with insulin or other antidiabetic agents for changes in glycemic control and adjust doses of these medications accordingly. Octreotide alters the balance between the counter-regulatory hormones of insulin, glucagon, and growth hormone, which may result in hypoglycemia or hyperglycemia. The hypoglycemia or hyperglycemia which occurs during octreotide acetate therapy is usually mild, but may result in overt diabetes mellitus or necessitate dose changes in insulin or other hypoglycemic agents. In patients with concomitant type1 diabetes mellitus, octreotide is likely to affect glucose regulation, and insulin requirements may be reduced. Symptomatic hypoglycemia, which may be severe, has been reported in type 1 diabetic patients. In Type 2 diabetes patients with partially intact insulin reserves, octreotide administration may result in decreases in plasma insulin levels and hyperglycemia.
Pasireotide: (Moderate) Monitor blood glucose levels regularly in patients with diabetes, especially when pasireotide treatment is initiated or when the dose is altered. Adjust treatment with antidiabetic agents as clinically indicated. Pasireotide inhibits the secretion of insulin and glucagon. Patients treated with pasireotide may experience either hypoglycemia or hyperglycemia.