Burn injuries very common. Most burns are limited to an extremity. Extensive burns/ burn trauma can be life-threatening or result in long-lasting complications. Bad burns can result in fibroproliferative scarring, skin contractures, or chronic wounds that take weeks or months to heal.
Burn injuries are highly patient-specific due to the wound-specific differences, such as general health status, age, immune status, genetics, burn depth and surface area.
The goal is to prevent a bacterial or other microbial super-infection, which can complicate wound healing, resulting in prolonged inflammation and delayed re-epithelialization.
Although mortality/death is decreasing due to innovations in burn care, morbidity/negative impacts on your life from post-burn deformities continues to be a challenge.
Here are the key things that should be done in any burn:
1. Make sure patient is safe and not near live electrical wires or water with a down power line. Be sure you are going to be safe rescuing the person or call 911 to get help.
2. Turn off all sources of the burn.
3. BURN WOUND MANAGEMENT |
a. Gently clean and apply a sterile guaze or very clean bandage if do not have anything sterile.
b. If it is a very dirty burn, clean with
Chronic wounds and severe burns are diseases responsible for severe morbidity and even death. Wound repair is a crucial process and tissue regeneration enhancement and infection prevention are key factors to minimize pain, discomfort, and scar formation. The aim of this work was the development of lipid nanoparticles (solid lipid nanoparticles and nanostructured lipid carriers [NLC]), to be loaded with eucalyptus or rosemary essential oils and to be used, as medical devices, to enhance healing of skin wounds. Lipid nanoparticles were based on natural lipids: cocoa butter, as solid lipid, and olive oil or sesame oil, as liquid lipids. Lecithin was chosen as surfactant to stabilize nanoparticles and to prevent their aggregation. The systems were prepared by high shear homogenization followed by ultrasound application. Nanoparticles were characterized for physical-chemical properties, bioadhesion, cytocompatibility, in vitro proliferation enhancement, and wound healing properties toward normal human dermal fibroblasts. Antimicrobial activity of nanoparticles was evaluated against two reference microbial strains, one of Staphylococcus aureus, the other of Streptococcus pyogenes. Finally, the capability of nanoparticles to promote wound healing in vivo was evaluated on a rat burn model. NLC based on olive oil and loaded with eucalyptus oil showed appropriate physical-chemical properties, good bioadhesion, cytocompatibility, in vitro proliferation enhancement, and wound healing properties toward fibroblasts, associated to antimicrobial properties. Moreover, the in vivo results evidenced the capability of these NLC to enhance the healing process. Olive oil, which is characterized by a high content of oleic acid, proved to exert a synergic effect with eucalyptus oil with respect to antimicrobial activity and wound repair promotion.

Polyhexamethylene guanidine or apply over-the-counter (OTC) Omnicide Antimicrobial Gel
c. If it is a severe burn, call 911 or go to ER or local Burn Center
d. If mild follow these general guidelines:
1) Keep area clean and covered with sterile guaze lightly covered.
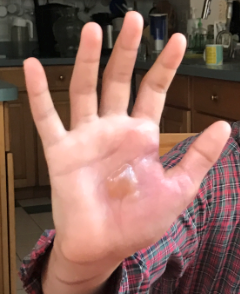
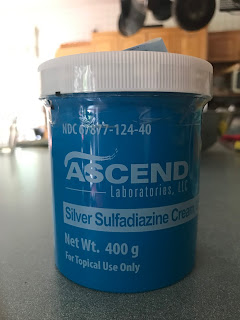
2) Silver sulfadiazine was considered a mainstay treatment for many years (I still use it for burns at home); however, two recent Cochrane reviews showed an increased rate of burn wound infection, poorer healing outcomes, and longer hospital stay when compared with biosynthetic, silicone-coated, and silver dressings or skin substitutes.(See Ref 3, 4)
Mafenide acetate is bactericidal and has the added advantage of better penetration of burn eschar 98,185; it is particularly useful in treating burns over auricular or nasal cartilage.
Burns treated with hydrogels showed a trend toward healing more quickly than with other dressings.184
A review of studies of topical treatments for facial burns showed that skin substitutes such as human cadaver allograft healed faster and with less pain compared with bacitracin or silver sulfadiazine.186,187
Here is a quick guide on how to clean wounds best:
General Principles |
|
Initial burn management begins with an assessment of the location, depth, and extent of the burn. The American Burn Association has established guidelines for referral to a burn center. Any patient being transferred to a regional burn center should have a simple dry dressing to keep the site warm and clean, avoid delaying transport, and avoid obscuring burn depth evaluation at the receiving institution.180
|
|
Deep partial-thickness burns are those that extend into the reticular dermis. In the absence of infection, they typically require 3 to 8 weeks to heal, with significant scarring.181 Full-thickness burns extend into the subcutaneous tissue; damage to the adnexal structures prevents spontaneous healing. Deep partial- or full-thickness burn should undergo early excision and grafting to reduce hypertrophic scarring (Fig. 4). In mixed-depth burns, a 5- to 7-day course of topical therapy will allow enough time for any spontaneous healing to occur.180
|
|
Débridement is performed at the fascial level or tangentially. Fascial débridement loses less blood, is faster to perform, and leaves a well-vascularized fascial bed that easily accepts a skin graft. It is best used in large burns but sacrifices some healthy tissue and leaves an unaesthetic contour 181 (Fig. 7). Tangential excision removes only the damaged tissue. Tangential excision is typically performed with a Weck or Goulian blade for small or irregularly contoured areas, and a Watson blade for larger areas
|
Burn Wound Dressings |
|
Silver sulfadiazine was considered a mainstay treatment for many years; however, two recent Cochrane reviews showed an increased rate of burn wound infection, poorer healing outcomes, and longer hospital stay when compared with biosynthetic, silicone-coated, and silver dressings or skin substitutes.(See Ref 3, 4) Mafenide acetate is bactericidal and has the added advantage of better penetration of burn eschar 98,185; it is particularly useful in treating burns over auricular or nasal cartilage. Burns treated with hydrogels showed a trend toward healing more quickly than with other dressings.184 A review of studies of topical treatments for facial burns showed that skin substitutes such as human cadaver allograft healed faster and with less pain compared with bacitracin or silver sulfadiazine.186,187
|
Silver-Impregnated Dressings |
|
Silver has wide-reaching antimicrobial properties against bacteria, fungi, and viruses, including methicillin-resistant Staphylococcus aureus. The highly reactive, negatively charged silver ion binds to DNA and RNA, preventing cellular replication.165,166 Silver sulfadiazine and silver nitrate have long been used to reduce infection in burns. More recently, products containing silver nanoparticles have become popular for treating open wounds and chronic ulcers. Recent Cochrane reviews have failed to demonstrate high-level evidence of benefit from silver-containing dressings in either preventing or treating infected wounds.167,168 Pressure ulcers treated with silver-based dressings have demonstrated a faster reduction in area.132 There is little evidence to support the use of silver dressings in diabetic foot ulcers.169
Systemic antibiotics do not reduce the incidence of burn wound infection or all-cause mortality.182 Targeted prophylaxis with trimethoprim-sulfamethoxazole may play a role in helping prevent pneumonia, based on results of a small trial.183 Increasing antibiotic resistance is of paramount concern when administering a systemic prophylactic antibiotic. |
References:
1. Plast Reconstr Surg. 2017 Jul;140(1):201e-216e. doi: 10.1097/PRS.0000000000003486.
Evidence-Based Medicine: Wound Management.
2.
3.
|
Barajas-Nava LA, López-Alcalde J, Roqué i Figuls M, Solà I, Bonfill Cosp X. Antibiotic prophylaxis for preventing burn wound infection. Cochrane Database Syst Rev. 2013;6:CD008738.
|
4.
|
Wasiak J, Cleland H, Campbell F, Spinks A. Dressings for superficial and partial thickness burns. Cochrane Database Syst Rev. 2013;3:CD002106.
|
5.
Int J Nanomedicine. 2017 Dec 27;13:175-186. doi: 10.2147/IJN.S152529. eCollection 2018.
Essential oil-loaded lipid nanoparticles for wound healing.
Saporito F1, Sandri G1, Bonferoni MC1, Rossi S1, Boselli C1, Icaro Cornaglia A2, Mannucci B3, Grisoli P1, Vigani B1, Ferrari F1.
Author information
- 1
- Department of Drug Sciences, University of Pavia, Pavia.
- 2
- Department of Public Health, Experimental and Forensic Medicine, University of Pavia, Pavia.
- 3
- Centro Grandi Strumenti, University of Pavia, Pavia, Italy.
Abstract
6.
Consensus Guidelines
Free Access
Consensus on Wound Antisepsis: Update 2018Kramer A.a · Dissemond J.c · Kim S.b · Willy C.d · Mayer D.e · Papke R.a · Tuchmann F.f · Assadian |
Int J Burns Trauma. 2017; 7(7): 142–146.
Published online 2017 Dec 20.
PMCID: PMC5768930
Treatment in the healing of burns with a cold plasma source
Introduction
Thermal burns have always been injuries caused by accidents, being of greater incidence in children and older adults. Surface burns or grade 1 burns are usually treated conservatively because the skin has a potential for reepithelialization, contrary to burns from grade 2 to grade 4 burns, which some of them have mixed patterns, or dermal lesions are deep. These pose an aesthetic and functional risk for the patient and end up compromising their life if they are extensive [1,2]. There is an urgent medical need not satisfied with new treatments for wounds and burns infections caused by different types of bacteria [3,4]. Among the results of research carried out in academic, clinical and industrial settings it can be mentioned: ultrasound [5], Laser [6] antimicrobial [7], negative pressure [8], micrografting [9], Colistin [10], etc.
Plasma medicine is an interdisciplinary field based on the exploit of non-thermal atmospheric-pressure plasma (cold plasma) [11,12], which has been investigated and developed by research groups, institutions, and laboratories worldwide. The plasma medicine potential has been applied in bacteria inactivation [13] and in vitro cancer treatment [14–16], likewise, in the living tissues [17,18] without causing damage due to the plasma temperature is below 40°C. The cold plasma produced at atmospheric pressure consists of charged particles, reactive species of both oxygen and nitrogen, and free radicals.
The cold plasmas of helium and/or argon have been tested in a preclinical environment in studies carried out at the Plasma Physics Laboratory of the National Institute of Nuclear Research [19]. They were applied in an experimental bio-model (laboratory mice of strain Balb/c), which were wounded with a length of ~1 cm and a depth of ~0.5 cm by a scalpel. Over the wound were applied three treatments using an argon plasma and subsequently three treatments with helium plasma, achieving accelerate healing process with the natural one [19]. This is because plasma is a potent generator of RNS/ROS species promoters of sterilization and tissue regenerators [19,20]. By means combining these plasmas are activated the coagulation proteins and promoted the activation and formation of the platelet of the fibrin filaments [21].
Investigations related to the application of cold plasma in humans are being carried out in an incipient way [22,23]. In this sense, we present in this paper a case report of a person who suffered skin burns produced by boiling oil on the inner part of a thigh and the lower part of a shin. The objective of the application of cold plasma was to take advantage of the bactericidal effect of this, as well as the rapid generation of the epithelium and the anti-inflammatory process.
Materials and methods
For the helium plasma application, the parameters reported in previous work with laboratory animals by García-Alcantara [19] were considered. So, the RF generator was 13.56 MHz coupled to a capacitor-inductor-capacitor circuit, the power applied to the plasma needle reactor was 10 W, in the treatments a 0.025 Ls-1 of helium was used, and the time-period in each session lasted 180 seconds, the distance between the needle-type reactor and the wound was 5 mm. Only two treatments were applied in one day with separation on four hours, and a surgical cleaning was performed before each treatment.
The here reported case was conducted according to the Helsinki II Declaration and the International Standard on Clinical Investigation of Medical Devices in Human Subjects. The protocol was approved by the ethics in research and research in health committees from the ISSEMYM medical center. Also, the written informed consent of the patient for the application of the treatment, the use, and publication of the information and photographs obtained.
Results and discussion
59-year-old male reports that is a man clinically healthy and suffers by burns produced three days before. These burns were caused by boiling oil and are shown in (Figure 1A) over a shin with a 15 cm2 of damage area and (Figure 1B) a thigh with a total damaged area of 79 cm2, and of this, the area covered by the crust is of 9 cm2. In these figures, you can see a slight epithelization.
The burned patient reports that he has severe pain; also that it is observed in both wounds a reddish color with blisters and inflammation. For this reason, both can be classified as burn wounds of the second degree. Besides, the patient reports that as treatment was applied the ointment with Nitrofurazone for three days.
Subsequently, the patient came back to the hospital, and it was decided to apply the treatment using a helium cold plasma by means of a needle-type reactor with the patient informed consent. A first treatment was applied with a duration of three minutes in each one of the wounds, and with the objective of eliminating the exudates fluid in the wound, it is cleaned with a surgical soap and saline solutions, before the cold application in plasma. After three hours of treatment, the appearance of the wound is shown in Figure 2. The patient reports that he no longer had non-itching pain and that he was able to withstand the clothing perfectly, as well as an increment in the epithelialization of the wound. There is no inflammatory process, which according to Farina et al. [24] is convenient for patients with burns. It is convenient indicating that the plasma process is a surface treatment and does not act on the already formed crusts, this is observed in both wounds of Figure 2.
After three hours of the first treatment with the cold plasma, it is applied for the second time on both wounds and again for three minutes in each of them. The patient returns the next day after 16 hours after the second treatment was applied, the results are shown in Figure 3. First, the patient reports having no discomfort except in the crusts that have a little itch, in particular, the crust area was not modified and remained in the 9 cm2. Also, there is a process of reepithelialization of both wounds and no longer bacterial presence.
Increased levels of free radicals generated by the cold plasma procedure may potentiate the process of wound reepithelialization, aiding the promotion of angiogenesis and influencing the bactericidal capacity of neutrophils and macrophages.
Conclusion
This new procedure for the treatment of burn wounds by the cold plasma can significantly assist in wound healing. Also, burn injuries can be directly treated since the cold plasma generates free radicals during the process preventing the infection of the wound. At the same time that the process of reepithelialization of the wounds presented in this case report did not show any inflammation effect. Possibly with the application of cold plasma early in lesions caused by burn can prevent serious complications thereof, since it can decrease the release of inflammatory mediators and bacterial colonization of wounds.
Acknowledgements
The authors appreciate the photographs and information shared by the patient. Likewise, we thank the participation of the nurse MG Navarrete-Granados and the technicians MT Torres-Martínez, P Angeles-Espinosa, I Contreras-Villa, M Lugo-Hernández in the construction of the different equipment systems used in this project.
References
1. Li H, Tan J, Zhou J, Yuan Z, Zhang J, Peng Y, Wu J, Luo G. Wound management and outcome of 595 electrical burns in a major burn center. J Surg Res. 2017;214:182–189. [PubMed]
2. Wallace HJ, Fear MW, Crowe MM, Martin LJ, Wood FM. Identification of factors predicting scar outcome after burn in adults: a prospective case-control study. Burns. 2017;43:1271–1283. [PubMed]
3. Rowan MP, Cancio LC, Elster EA, Burmeister DM, Rose LF, Natesan S, Chan RK, Christy RJ, Chung KK. Burn wound healing and treatment: review and advancements. Crit Care. 2015;19:243.[PMC free article] [PubMed]
4. Oryan A, Alemzadeh E, Moshiri A. Burn wound healing: present concepts, treatment strategies and future directions. J Wound Care. 2017;26:5–19. [PubMed]
5. Silva-Fantinati M, Oliveira-Mendonça DE, Monteiro-Fantinati AM, Flamarion-dos Santos B, Oliveira-Reis JC, Lopes-Afonso C, Clare-Vinaud M, Lino-Júnior R de S. Low intensity ultrasound therapy induces angiogenesis and persistent inflammation in the chronic phase of the healing process of third degree burn wounds experimentally induced in diabetic and non-diabetic rats. Acta Cir Bras. 2016;31:463–471.[PubMed]
6. Brassolatti P, Bossini PS, Derencio Oliveira MC, Kido HW, Tim CR, Almeida-Lopes L, da Silva de Avo LR, Araujo-Moreira FM, Parizotto NA. Comparative effects of two different doses of lowlevel laser therapy on wound healing third-degree burns in rats. Microsc Res Tech. 2016;79:313–320. [PubMed]
7. Shafaei S, Dörrstein J, Guggenbichler JP, Zollfrank C. Cellulose acetate-based composites with antimicrobial properties from embedded molybdenum trioxide particles. Lett Appl Microbiol. 2017;64-1:43–50.
8. El-Sabbagh AH. Negative pressure wound therapy: an update. Chin J Traumatol. 2017;20:103–107.[PMC free article] [PubMed]
9. Rode H, Martinez R, Potgieter D, Adams S, Rogers AD. Experience and outcomes of micrografting for major paediatric burns. Burns. 2017;43:1103–1110. [PubMed]
10. Zhu C, Zhao J, Kempe K, Wilson P, Wang J, Velkov T, Li J, Davis TP, Whittaker MR, Haddleton DM. A hydrogel-based localized release of colistin for antimicrobial treatment of burn wound infection. Macromol Biosci. 2017:17.
11. Graves DB. Low temperature plasma biomedicine: a tutorial review. Phys Plasmas. 2014;21:e080901.
12. Laroussi M. Low-temperature plasma jet for biomedical applications: a review. IEEE Trans Plasma Sci. 2015;3:703–712.
13. Pignata C, D’Angelo D, Fea E, Gilli G. Review on microbiological decontamination of fresh produce with nonthermal plasma. J Appl Microbiol. 2017;122:1438–1455. [PubMed]
14. Ratovitski EA, Cheng X, Yan D, Sherman JH, Canady J, Trink B, Keidar M. Anti-cancer therapies of 21st century: novel approach to treat human cancers using cold atmospheric plasma. Plasma Process Polym. 2014;11:1128–1137.
15. Trink B, Keidar M, Canady J, Shamai Y, Tzukerman M. The effect of cold atmospheric plasma treatment on cancer stem cells. Plasma Med. 2015;5:17–26.
16. Reiazi R, Akbari ME, Norozi A, Etedadialiabadi M. Application of cold atmospheric plasma (CAP) in cancer therapy: a review. Int J Cancer Manag. 2017;10:e8728.
17. Hung YW, Lee LT, Peng YC, Chang CT, Wong YK, Tung KC. Effect of a nonthermal-atmospheric pressure plasma jet on wound healing: an animal study. J Chin Med Assoc. 2016;79:320–328. [PubMed]
18. Kubinova SA, Zaviskova K, Uherkova L, Zablotskii V, Churpita O, Lunov O, Dejneka A. Non-thermal air plasma promotes the healing of acute skin wounds in rats. Sci Rep. 2017;7:e45183.
19. García-Alcantara E, López-Callejas R, Morales-Ramírez PR, Peña-Eguiluz R, Fajardo-Muñoz R, Mercado-Cabrera A, Barocio SR, Valencia-Alvarado R, Rodríguez-Méndez BG, Muñoz-Castro AE, de la Piedad-Beneitez A, Rojas-Olmedo IA. Accelerated mice skin acute wound healing Z by combined treatment of argon and helium plasma needle. Arch Med Res. 2013;44:169–177. [PubMed]
20. Schmidt A, Dietrich S, Steuer A, Weltmann KD, von Woedtke T, Masur K, Wende K. Non-thermal plasma activates human keratinocytes by stimulation of antioxidant and phase II pathways. J Biol Chem. 2015;290:6731–6750. [PMC free article] [PubMed]
21. Zhu G, Wang Q, Lu S, Niu Y. Hydrogen peroxide: a potential wound therapeutic target? Med Princ Pract. 2017;26:301–308. [PMC free article] [PubMed]
22. Isbary G, Zimmermann JL, Shimizu T, Li YF, Morfill GE, Thomas HM, Steffes B, Heinlin J, Karrer S, Stolz W. Non-thermal plasma-more than five years of clinical experience. Clin Plasma Med. 2013;1:19–23.
23. Horiba M, Kamiya T, Hara H, Adachi T. Cytoprotective effects of mild plasma-activated medium against oxidative stress in human skin fibroblasts. Sci Rep. 2017;7:e42208.
24. Farina JA Jr, Rosique MJ, Rosique RG. Curbing inflammation in burn patients. Int J Inflam. 2013;2013:715645. [PMC free article] [PubMed]