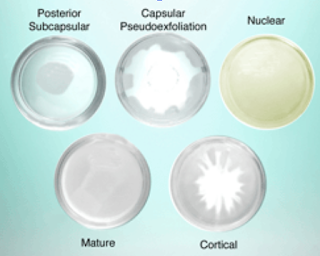
Types of Cataracts (ie, the “pillow” inside the capsule or “pillowcase”)
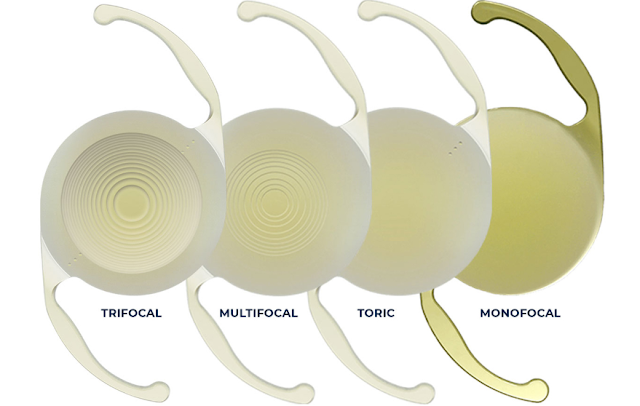
The oldest type of implants are the Monofocals, which insurance still covers, but these only give you one plane of vision, usually we correct for distance. These have the least amount of halos and glare but more than 95% need glasses for intermediate and reading after these implants.
The next generation is the Multifocal Implants. These have a higher chance of getting a patient glasses-free for distance and intermediate but halos and glare after cataract surgery were significant and the trade-off was not worth it for most patients with the Restor and Rezoom Multifocal IOLs.
Accommodating IOLs like the Crystalens kept halos and glare to a minimum but again did not give patients great reading vision over time as the capsule (ie, “the pillowcase”) often would opacity.
The next generation was the Extended Depth of Focus implant or the Symfony implant, which patients loved but the reading vision was not great and often patients still needed reading glasses.
The newest implant is the Trifocal PanOptix intraocular lens (IOL), which the FDA approved in August 2019, though it has been in use in Europe since June 2015. PanOptix uses a quadrifocal (4 foci) design and uses proprietary optical technology, ENLIGHTEN, to redistribute the focal point at 120 cm to the distance focal point for maximum performance. This results in 2-step heights that are equal to 2 add powers/2 focal points (plus the distance from the base curve).
See https://www-ncbi-nlm-nih-gov.proxy1.library.jhu.edu/pmc/articles/PMC6727923/
Light is split to 3 foci (distance: ∞, intermediate at 60 cm, and near at 40 cm). The 4.5 mm non-apodized, diffractive zone allows high light utilization, transmitting 88% of light to the retina at a 3.0 mm pupil size, and provides optimized performance in a wide range of lighting conditions due to low dependence on the pupil size. This light energy is distributed 25% each for near and intermediate and 50% for distance vision. When light is split between distance, reading, and near, it means that vision quality will be affected with more halos and glare than a Monofocal and that contrast sensitivity may be an issue. For most patients, noticeable halos, glare, and decreased contrast sensitivity will not be bothersome as their brains can adjust to it well. These patients love the new implants, particularly the PanOptix. See data below on the percentage of patients that love the PanOptix. ** https://www-ncbi-nlm-nih-gov.proxy1.library.jhu.edu/pmc/articles/PMC6727923/
Thus to help a patient see 20/20 at distance, intermediate, and reading after cataract surgery requires glasses, like Progressive glasses or 3 separate glasses OR requires special implants, such as the Trifocal-PanOptix intraocular lens (IOL) and Femtosecond Laser-Assisted Cataract Surgery which also helps decrease corneal astigmatism by making small microscopic cuts in the cornea. While there is not a 100% guarantee a patient who chooses both the Pan-Optix and Femtosecond Laser-Assisted Cataract surgery will be glasses-free, the FDA data and many publications in Europe and the US have shown over 90% chance of being glasses-free for distance and intermediate and over an 87% chance of being glasses-free for reading with the PanOptix IOL. Our experience agrees with these studies: the vast majority of patients love this implant and would choose it again. For patients who are jewelers or do very close work, they have a higher chance of needing reading glasses even with the PanOptix. Some patients who want to be completely glasses-free for reading would have to choose intraocular implants in 1 or both eyes that are between -1.75-2.50D but then would need glasses for intermediate and distance.
References:
1.
This study used a short quality of vision (QoV) questionnaire (19 items) to assess patient-reported outcomes based on presence of visual disturbances and lifestyle activities, choice of IOL, and spectacle independence. Complete spectacle independence was achieved by 96% of patients with only 1 patient (1/27) reporting the use of spectacles for far distance. In all, 93% of patients reported experiencing an optical phenomena (89% halos, 11% glare, 7% double vision, 4% each ghosting and distorted vision).10 Although the reported incidence for far distance halos was high, patients reported that it was not bothersome. In all, 81% of patients responded that they would choose the same IOL again and would recommend it to others. For daily life activities, patients rated (score range: 1 = good to 6 = bad) a good mean score for the quality of uncorrected vision of 2.1 ± 0.54 for distance activities (car driving, TV, theatre, among others), and of 1.8 ± 0.10 for near and intermediate distance (cooking, computer, musical instrument, newspaper).10
2.Extended Depth of Focus (EDOF) IOL TECNIS Symfony (Abbott Medical Optics, Santa Ana, CA) was launched in 2014.
AcrySof IQ PanOptix Model TFNT00 (Alcon Laboratories, Fort Worth, TX) is a quadrifocal, presbyopia-correcting IOL first launched in Europe in 2015, that uses the ENhanced LIGHT ENergy (ENLIGHTEN; Alcon Laboratories, Fort Worth, TX) optical technology. It only became available in the USA in September 2019.
-The PanOptix IOL is designed to have an intermediate focal point of 60 cm (arms-length), a more natural and comfortable working distance to perform functional tasks on computers, laptops, mobiles, among others.
– non-apodized
– high (88%) utilization of light energy
-low dependence on pupil size in all lighting conditions
-a more comfortable near-to-intermediate range of vision than traditional trifocal IOLs.
FineVision Micro F (PhysIOL, Liege, Belgium) was first trifocal IOL introduced in Europe in 2010 but is not available in the USA as of 2019. Has an intermediate focal point of 80 cm.
AT LISA tri 839MP (Carl Zeiss Meditec AG, Jena, Germany) is second trifocal IOLs introduced in Europe in 2012 but is not available in the USA as of 2019. Has an intermediate focal point of 80 cm.
3. https://www.accessdata.fda.gov/cdrh_docs/pdf4/P040020S087C.pdf
1
PATIENT
INFORMATION
BROCHURE
AcrySof® IQ PanOptix® Trifocal IOL
Model TFNT00
AcrySof® IQ PanOptix® Toric Trifocal IOLs
Models TFNT30, TFNT40, TFNT50, TFNT60
Alcon Laboratories, Inc.
6201 South Freeway
Fort Worth, Texas 76134-2099 USA
Toll free (800) 757-9785
2
Table of Contents
Introduction …………………………………………………………………………………………………………………… 3
What is a cataract? …………………………………………………………………………………………………………. 3
What is corneal astigmatism?…………………………………………………………………………………………… 3
What is an Intraocular Lens (IOL)?…………………………………………………………………………………….. 3
What is the surgical procedure to restore my vision?………………………………………………………….. 4
Potential Risks Associated with Cataract Surgery ……………………………………………………………….. 4
What types of IOLs are available for this procedure? ………………………………………………………….. 5
Monofocal IOLs………………………………………………………………………………………………………………. 5
Monofocal Toric IOLs………………………………………………………………………………………………………. 5
Multifocal IOLs……………………………………………………………………………………………………………….. 5
Multifocal Toric IOLs……………………………………………………………………………………………………….. 5
Alcon AcrySof® IQ PanOptix® Trifocal IOLs…………………………………………………………………………. 5
Potential Side Effects Associated with AcrySof® IQ PanOptix® Trifocal IOLs…………………………… 6
Clinical Study Results………………………………………………………………………………………………………..6
Warnings……………………………………………………………………………………………………………………… 11
Precautions………………………………………………………………………………………………………………….. 12
Postoperative Care Instructions ……………………………………………………………………………………… 12
Key points to remember regarding your choice ………………………………………………………………… 12
3
PATIENT INFORMATION BROCHURE
Alcon AcrySof® IQ PanOptix® Trifocal Intraocular Lens (IOL)
Introduction
This brochure is intended to help you and your surgeon decide what type of intraocular lens
(IOL) to choose for your cataract surgery. If the lens in your eye gets so cloudy that it makes
your vision worse, it is called a cataract. Cataract surgery can restore good vision by removing
the cloudy lens from your eye and replacing it with a clear artificial lens or IOL. Your surgeon
will explain the risks and possible benefits of cataract surgery and will describe the different
kinds of IOL that are available. This brochure can help you to decide whether an Alcon
AcrySof® IQ PanOptix® Trifocal IOL would be a good choice for you. You can also read about
other possible choices in the section called “What types of IOLs are available for this
procedure?”.
What is a cataract?
Your eye functions much like a camera. Your natural lens focuses images onto the back of your
eye so you can see clearly, much like the lens of a camera focusing images onto film for a clear
picture. At birth, your natural lens is clear. However, as you age, the lens may begin to gradually
become “cloudy.” This condition is called a cataract, and is usually a result of the natural aging
process. As the lens becomes cloudier, your quality of vision may decrease.
A cataract can progress until eventually there is a complete loss of vision in your eye. Surgery is
the only way a cataract can be removed. You should consider surgery when cataracts cause
enough loss of vision to interfere with your daily activities.
What is corneal astigmatism?
Astigmatism is a focusing error in the eye that results in blurred distance and/or near vision. In
a normal eye, the cornea (front of the eye) has a round shape (like a basketball); therefore, the
light rays entering the eye focus at a single point on the back of the eye (retina) to form a clear
image. In an eye with corneal astigmatism, the cornea has an oblong shape (like an American
football). As a result, the light rays do not focus at the same point on the retina and parts of an
object may not appear clear. During your eye examination, your eye doctor will be able to tell
you if you have corneal astigmatism.
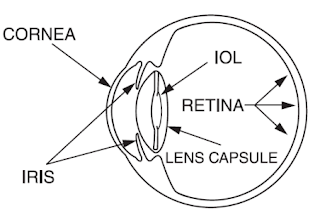
What is an Intraocular Lens (IOL)?
An intraocular lens, commonly referred to as an IOL, is an artificial lens that is implanted into
the eye to replace the natural lens when a cataract is removed. Figure 1, below, shows the basic
parts of the human eye with an IOL.
In general, lOLs have two basic features. The optic portion is the round part of the IOL that
focuses an image onto the back of your eye. Two arm-like structures called haptics are attached
to the edge of the optic. The haptics help to maintain the location of the IOL in the eye.
4
Figure 1 – Drawing of the Human Eye with an IOL
What is the surgical procedure to restore my vision?
After you and your eye doctor have decided that you will have your cataract removed, your eye
will be measured (commonly referred to as biometry). This will help to determine the suitable
IOL for you that will be placed in your eye during surgery.
When you arrive for surgery, you will be given eye drops and perhaps medicines to help you
relax. Cataract surgery techniques vary widely. However, the eye is always numbed to make the
operation painless. To perform surgery, your eye doctor will use a microscope to have a
magnified view of your eye. Your natural lens sits in a bag-like structure called the lens capsule.
The lens capsule is located just behind the colored part of your eye (iris). A small incision is
made in the outer surface of the eye. Through this opening, the eye doctor removes the center
part of the front of the lens capsule and then inserts a tiny instrument to break-up and remove
the cataract. An IOL is then placed into the capsule to replace your natural lens that your eye
doctor has just removed. The IOL will focus light inside the eye to allow you to see. The surgeon
will usually place a shield over your eye after surgery. You will be ready to go home after a short
stay in the outpatient recovery area. Plan to have someone else drive you home.
Potential Risks Associated with Cataract Surgery
As with any surgery, there are risks and potential problems associated with routine cataract
surgery and IOL placement. General surgery risks include reactions to medicines, bleeding,
infection, inflammation, redness, scratchiness of the eye, sensitivity to light, and increased
eye pressure. There is a small chance that your vision could be made worse by the
operation. Please discuss these general risks associated with cataract surgery with your eye
doctor.
5
What types of IOLs are available for this procedure?
There are many different lOLs to choose from. Some of the main types are described below. Your
eye doctor will discuss your options, including AcrySof® IQ PanOptix® Trifocal IOLs and other IOLs.
Discuss all of your IOL options with your eye doctor.
Monofocal IOLs
A monofocal IOL is designed to provide clear distance vision. This means you will usually be able
to see objects far away, but there is still a small chance that you may need glasses for distance
vision. You will most likely need glasses for near vision activities such as reading, writing, and
sewing, as well as intermediate vision activities such as applying makeup or shaving, and working
on a computer. These lenses do not correct for corneal astigmatism. Patients who have larger
amounts of corneal astigmatism and who are implanted with a monofocal IOL may need glasses
for distance vision.
Monofocal Toric IOLs
A monofocal toric IOL is designed to provide clear distance vision and correct corneal
astigmatism. There are different models of monofocal toric IOLs for varying levels of corneal
astigmatism. With a monofocal toric IOL, you will be able to see objects far away, but there is
still a small chance that you may need glasses for distance vision. However, you will most likely
still need glasses for near distance activities such as reading, writing, sewing as well as
intermediate distance activities such as viewing a cell phone, applying makeup or shaving or
working on a computer.
Multifocal IOLs
Multifocal IOLs allow for clear distance vision (e.g., for watching children playing in the
backyard). The design of the IOL also allows for better near (reading) and intermediate
(computer work) vision than a monofocal lens would provide. Different multifocal IOLs have
different optical strengths for near vision. There is a chance you may still need glasses for
distance, intermediate, and/or near vision. These lenses do not correct for corneal astigmatism.
Multifocal Toric IOLs
In addition to the benefits of the Multifocal IOLs, the Multifocal Toric IOLs provide corneal
astigmatism correction. Most Multifocal IOLs are available in a non-toric and a toric version to
allow for the full range of patients without or with pre-existing astigmatism. Like the other types
of IOLs, there is a chance you may still need glasses for distance, intermediate, and/or near vision
with a Multifocal Toric IOL.
Alcon AcrySof® IQ PanOptix® Trifocal IOLs
The AcrySof® IQ PanOptix® Trifocal IOL is a type of multifocal IOL and has the same basic shape
and identical materials as Alcon AcrySof® monofocal and monofocal toric IOLs. Like a monofocal
lens, the purpose of the AcrySof® IQ PanOptix® Trifocal IOL is to focus images clearly onto the
back of your eye (retina) to allow clear vision after the cataract removal. In addition, the center
6
of the AcrySof® IQ PanOptix® Trifocal IOL allows for better near (reading) vision and intermediate
(computer work) vision versus what a monofocal lens wouldprovide.
The AcrySof® IQ PanOptix® Trifocal IOL is offered in five models (TFNT00, TFNT30, TFNT40,
TFNT50, TFNT60). All models provide similar distance, better intermediate, and better near
vision compared to monofocal IOLs.
The most appropriate model will be chosen by your surgeon based on the amount of your
corneal astigmatism, including Model TFNT00 if you have no corneal astigmatism (this model
does not correct for corneal astigmatism).
There is a chance that you still may need glasses for distance, intermediate, and/or near vision.
You will get the full benefit of the AcrySof® IQ PanOptix® Trifocal IOL when it is placed in both
eyes. Please discuss with your eye doctor whether this is the right IOL for you.
Potential Side Effects Associated with AcrySof® IQ PanOptix® Trifocal
IOLs
Due to the design of multifocal IOLs, there are some side effects that can be associated with the
AcrySof® IQ PanOptix® Trifocal IOL models. These may be worse than with a monofocal IOL,
including visual disturbances such as glare, rings around lights, starbursts (rays around light
sources), and reduced contrast sensitivity (decrease in ability to distinguish objects from their
background, especially in dim lighting). These side effects may make it more difficult to see while
driving at night or completing tasks in low lighting conditions such as at night or in fog, or in a
dimly lit room after surgery as compared to before surgery.
Further, a toric IOL corrects astigmatism only when it is placed in the correct position in the eye.
There is a possibility that the toric IOL could be placed incorrectly or could move within the eye.
If the toric lens is not positioned correctly following surgery, the change in your astigmatism
correction by the IOL, along with any necessary correction with glasses, may cause visual
distortions. If the lens rotates in your eye, you may need additional surgery to reposition or
replace the IOL.
Clinical study results
A human clinical study comparing AcrySof® IQ PanOptix® Trifocal IOL Model TFNT00 (without the
toric feature for correcting corneal astigmatism) against a monofocal lens, the AcrySof Monofocal
IOL Model SN60AT was conducted in the United States. Important results from this study are
provided are described below:
Overall Impact on Vision:
The clinical study involved testing with both eyes as well as testing on each eye one at a time.
Results from are provided in Table 1.
7
Table 1. Comparison of Study Results between AcrySof® IQ PanOptix® IOL Model TFNT00 and
AcrySof® Monofocal IOL Model SN60AT at 6 months After Surgery.
PanOptix® IOL Monofocal IOL
Percentage of patients who
achieved approximately 20/25
or better vision*
Percentage of patients who achieved
approximately 20/25 or better vision*
One eye
tested alone
Both eyes tested
together
One eye
tested alone
Both eyes tested
together
Distance Vision without
glasses (driving, playing
golf, etc.)
72% 92% 84% 100%
Distance Vision with
glasses (driving, playing
golf, etc.)
98% 100% 99% 100%
Intermediate Vision
without glasses eyes
(computer work,
cooking, etc.) at
approximately 26 inches.
71% 94% 28% 51%
Intermediate Vision with
glasses for distance
(computer work,
cooking, etc.) at
approximately 26 inches.
81% 98% 7% 26%
Near Vision without
glasses (reading,
threading a needle, etc.)
at approximately 16
inches.
65% 92% 2% 9%
Near Vision with glasses
for distance (reading,
threading a needle, etc.)
at approximately 16
inches.
76% 96% 0% 0%
* On an eye chart, reading all the letters on the 20/25 line with no mistakes means you have 20/25 or better vision.
Reading the majority of the 20/25 line correctly means you have approximately 20/25 or better vision.
8
Need for Eyeglasses*: Patients were asked about how often they needed glasses overall and their
responses are presented in Table 2.
Table 2.Need for Eyeglasses*
Frequency Percentage of patients who reported wearing glasses Overall
PanOptix® IOL
129 patients
Monofocal IOL
114 patients
Never 80.5% 8.2%
* “Eyeglasses” also mean bifocals, “readers”, contact lenses or prescription sunglasses.
Adverse events: Collective serious adverse events in the eye for the AcrySof® IQ PanOptix®
Trifocal IOL and the AcrySof® Monofocal IOL Model SN60AT are presented in table 3.
Table 3.
PanOptix® IOL Monofocal IOL
4 out of 129 patients reported having serious adverse
events:
Adverse events related to cataract surgery but not the
PanOptix® IOL:
• One patient had swelling in the retina which
was treated with medication and recovered.
This patient also required a second surgical
procedure to reposition the IOL due to a tilted
IOL, which recovered after the surgery.
• One patient had a tear of the retina that
recovered without any treatment.
• One patient had vitreous (gelatinous tissue
filling the eyeball behind the lens) enter the
front part of the eye, which needed to be
removed with a second surgical procedure.
The patient recovered after surgery.
Adverse event related to PanOptix® IOL but not the
cataract surgery:
• One patient required a second surgery to
remove the IOL due to complaints of
dissatisfaction with level of vision. The patient
recovered after surgery.
2 out of 114 patients reported having serious adverse
events:
Adverse events not related to the Monofocal IOL or
cataract surgery:
• One patient had age-related macular
degeneration and needed medication injected in
both eyes to treat abnormal blood vessel growth
in the back of the eye. The patient recovered
after the procedure.
Adverse events related to cataract surgery but not the
Monofocal IOL:
• One patient needed a second surgical procedure
to remove the IOL from the eye because a tear
in the capsule (bag-like structure) holding the
IOL caused the IOL to not be centered in the eye.
The patient recovered after the surgery.
9
Contrast Sensitivity:
Contrast sensitivity, an important measure of visual function, is the ability to distinguish objects
from their background, especially in dim lighting. In patients who received the AcrySof® IQ
PanOptix® Trifocal IOL Model TFNT00, contrast sensitivity was well maintained, regardless of
lighting conditions or the presence of glare. Results of this study indicate that contrast sensitivity
was slightly worse in patients receiving the AcrySof® IQ PanOptix® Trifocal IOL Model TFNT00
compared to those who received the monofocal IOL.
Visual Disturbances:
Patients were asked “How Severe was your worst Experience?” Table 4 below shows the
number of patients who reported their visual disturbances such as glare, rings around lights,
starbursts to be severe. The rates of severe halos, starbursts, and glare were higher in the
PanOptix® IOL group compared to the Monofocal IOL group. Patients were also asked to rate
how much specific visual symptoms bothered them. Table 5 below shows the number of
patients who reported being most bothered (“Bothered very much”) by visual
disturbances. Note that fewer patients were most bothered by the visual disturbance (less
than 5%) than rated it severe.
Table 4. Rates of patients reporting their Visual Disturbances to be severe, per 100 patients, 6
months After Surgery
PanOptix® IOL Monofocal IOL
6 Months 6 Months
Halos (rings around lights) 13% 1%
Starbursts (rays around light
sources)
16% 2%
Glare 3% 2%
Blurred Vision (reduced
sharpness in vision)
0% 0%
Hazy Vision (reduced
contrast sensitivity)
0% 0%
Double Vision 0% 0%
Dark Areas 0% 0%
10
Table 5. Rates of patients reporting “Bothered very much” by certain Visual Disturbances, per
100 patients, 6 months After Surgery
PanOptix® IOL Monofocal IOL
6 Months 6 Months
Halos (rings around lights) 2% 1%
Starbursts (rays around light
sources)
5% 1%
Glare 2% 1%
Blurred Vision (reduced
sharpness in vision)
0% 2%
Hazy Vision (reduced
contrast sensitivity)
0% 1%
Double Vision 0% 0%
Dark Areas 0% 0%
Effect of Astigmatism remaining after cataract surgery
Some patients may have some level of astigmatism remaining after IOL placement, especially if
they had a lot of astigmatism before surgery or if their AcrySof® IQ PanOptix® Toric Trifocal IOL
was placed incorrectly or moved within the eye after surgery. The effect of this was studied by
artificially creating astigmatism for patients using glasses. As with other multifocal IOLs, patients
with large artificial levels of residual astigmatism showed reduced vision.
As with any multifocal toric IOL, if the IOL is not placed correctly in your eye or if the amount of
remaining astigmatism after the surgery was calculated incorrectly :
o Your may have poor vision
o You may need to wear eye glasses to see clearly (for far, intermediate, and near
distances)
o You may need a second surgical procedure to correct the position of your IOL
Other Clinical studies:
Alcon multifocal (AcrySof ReSTOR IOL Models MA60D3 and SA60D3) and multifocal toric IOLs
(AcrySof IQ ReSTOR +3.0 D Multifocal Toric IOL Models SND1T3 to SND1T6) have been clinically
studied. AcrySof® IQ PanOptix® Trifocal IOL and AcrySof® IQ PanOptix® Toric Trifocal IOL are
modifications of these multifocal models. Therefore, the study completed on the previous models
are applicable to AcrySof® IQ PanOptix® Trifocal IOLs with regards to the results described below.
A night driving simulation study was previously conducted on AcrySof ReSTOR IOL Models
MA60D3 and SA60D3. Patients who received Alcon multifocal and monofocal IOLs were asked to
assess the effects of various lighting conditions on their vision. The ability of multifocal IOL
patients to detect and identify road signs and hazards at night was similar to the monofocal IOL
patients under normal visibility conditions. Sign identification in fog and glare conditions were
more challenging for the multifocal IOL patients compared to monofocal IOL patients. The ability
to detect hazards was also lower for multifocal patients than for monofocal patients, especially
when glare was present.
11
Warnings
• As with other multifocal IOLs, there is a possibility that you may experience very
bothersome visual disturbances such as starbursts, halos and glare. This may cause you
to be dissatisfied to the point of requesting removal of the IOL.
• It may be more difficult to see while driving at night or completing tasks in low
lighting conditions such as at night or in fog, after surgery. Therefore, you should take
extra care when driving at night.
• Your vision may not be as good with a multifocal IOL if you have irregular astigmatism
(if before surgery it is determined that the front surface of your eye is irregular in
shape).
• Your vision may not be as good if you choose the non-Toric AcrySof® IQ PanOptix® Trifocal
IOL and have large amount of astigmatism before surgery and/or are expected to have a
large amount of astigmatism after surgery.
• Your vision may not be as good if you choose AcrySof® IQ PanOptix® Toric Trifocal IOL and
have a large amount of astigmatism after surgery.
• As with other IOLs, if there are unexpected results, there is a chance you may need to
continue wearing eye glasses or may need a second surgical procedure to reposition your
IOL.
• Contact your eye doctor immediately if you have any of the following symptoms after
surgery: a significant decrease in vision, a significant increase in pain, significant itching,
significant redness, watering of your eye, double vision persisting more than a few days,
significant eye discharge, and increased sensitivity to light. These symptoms could
indicate potential serious postoperative complications including, but not limited to, eye
infection, increased intraocular pressure, retinal detachment, wound leak, allergic
reaction to medications, or lens dislocation.
• Patients with pre-existing retinal problems that reduce their vision, such as macular
degeneration or diabetic edema, may not benefit from or may have a poorer visual
outcome following cataract surgery with multifocal IOL placement.
Please discuss all risks and benefits with your eye doctor before your surgery.
Precautions
• Before surgery, your eye doctor will check to see if you have any eye diseases or swelling.
Be sure to tell your eye doctor if you have any health conditions (e.g., breathing difficulties,
heart trouble, allergies, previous eye surgery) that may affect your surgery or vision.
• The safety and effectiveness of the AcrySof® IQ PanOptix® Trifocal IOL has not been
established in patients with certain eye conditions, such as glaucoma or diabetic retinopathy
(an increase in eye pressure or complications of diabetes in the eye). The outcome of
cataract surgery will depend on the health of your eye before surgery. You should tell your
eye doctor if you have been diagnosed as having amblyopia (lazy eye) or any other eye
disease.
• The capsule (bag-like structure) that your IOL is placed in may become cloudy after cataract
surgery. If this condition develops, it may affect your vision earlier if you receive the AcrySof®
12
IQ PanOptix® Trifocal IOL compared to someone who receives with a standard monofocal
IOL.
• AcrySof® IQ PanOptix® Toric Trifocal IOL have not been evaluated in a clinical study.
However, the effects of astigmatism remaining after the surgery has been studied
using simulation techniques. As with any multifocal toric IOL, you may need
eyeglasses to see clearly (for far, intermediate, and near distances) if you have a
large amount of astigmatism after surgery. You should avoid any activity that could
harm your eye while you are recovering from surgery. Your eye doctor will tell you
what activities you should avoid.
• Take all prescribed medicines and apply eye drops asinstructed.
You should tell your eye doctor of any eye problems or if you have been diagnosed with any eye
condition.
Postoperative Care Instructions
You will return home after surgery. Typically, your eye doctor will examine you the following
day. Your eye doctor will give you eye drops to speed up the healing process and to prevent
infection.
Your vision should improve within 4 to 6 weeks after cataract surgery. Many patients may see
better within 1 to 2 weeks or less. The specifics of surgery may be different for each individual.
Be sure to consult your eye doctor so you can fully understand the recovery process after the
cataract surgery. It may take you some time to get accustomed to your new IOL(s). Always
consult your eye doctor if you have any questions or concerns as a result of cataract surgery.
Key points to remember regarding your choice
• Monofocal, multifocal, including toric and non-toric IOLs can restore your vision following
cataract surgery.
• It is important to discuss your lifestyle or visual needs with your eye doctor to help select
the most suitable IOL for you.
• There is a greater chance of experiencing starbursts, halos and glare with a Multifocal IOL as
compared to a Monofocal IOL.
Thank you for considering the Alcon AcrySof® IQ PanOptix® Trifocal family of IOLs.
Alcon Laboratories, Inc.
6201 South Freeway
Fort Worth, Texas 76134-2099 USA
Comparison of Mix-and-Match Implanted Bifocal IOLs and Bilateral Implanted Trifocal IOLs After Femtosecond Laser-Assisted Cataract Surgery.
Abstract
PURPOSE:
METHODS:
RESULTS:
CONCLUSIONS:
Correlation and predictability of ocular aberrations and the visual outcome after quadrifocal intraocular lens implantation: a retrospective longitudinal study.
Author information
- 1
- Department of Ophthalmology, Show Chwan Memorial Hospital, Changhua, Taiwan. ao6u.3msn@hotmail.com.
- 2
- Department of Optometry, College of Medicine and Life Science, Chung Hwa University of Medical Technology, Tainan, Taiwan. ao6u.3msn@hotmail.com.
- 3
- Institute of Medicine, Chung Shan Medical University, Taichung, Taiwan.
- 4
- Department of Optometry, Chung Shan Medical University, Taichung, Taiwan.
- 5
- Department of Optometry, Yuanpei University of Medical Technology , Hsinchu, Taiwan.
- 6
- Department of Exercise and Health Promotion, Chung Chou University of Science and Technology, Changhua, Taiwan.
- 7
- Department of Medical Research, Chung Shan Medical University Hospital, Taichung, Taiwan.
- 8
- Department of Ophthalmology, Chang Gung Memorial Hospital, Linkou, Taiwan.
- 9
- Department of Medicine, Chang Gung University College of Medicine, Taoyuan, Taiwan.
- 10
- Department of Ophthalmology, Show Chwan Memorial Hospital, Changhua, Taiwan.
- 11
- Center for Tissue Engineering, Chang Gung Memorial Hospital, Linkou, Taiwan.
- 12
- Department of Ophthalmology, Chang Gung Memorial Hospital, Keelung, Taiwan.
- 13
- Department of Chinese Medicine, Chang Gung University, Taoyuan, Taiwan.