Update: A friend called me to say, her whole household of 8 had it & she swears by this product below. Though there are no randomized controlled studies to say it works, it did get good reviews. I would likely try this before getting an Rx. She got both & it took 2 days to be lice free. It saved her hundreds given the cheapest in her area for a professional treatment for her whole family was more than $400.
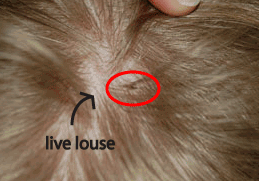
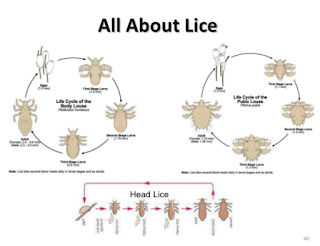
Head lice (Pediculus humanus capitis) is unfortunately very common and a pain to deal with. They cause scalp irritation and all kinds of social disruption issues (ie, the cancelling of a looked-forward-to Easter.) It can even cause poor sleep, excoriations that risk bacterial superinfection, and loss of school and even work days.
1. Widespread use of pyrethroids has precipitated their current ineffectiveness in the treatment of infestations due to wide spread resistance.
2. There is no published data to show Home remedies such as mayonnaise, and essential oils, have not been demonstrated to be safe or effective, and may carry potential for severe adverse events. They go on to say the below statement towards end. Still no good studies have been done in my opinion to fully rule out home remedies as an option in young kids.
3. Transmission of lice is from human head to muman head contact thru hands, brushes, combs, etc. head-to-head contact.
a. Eggs are laid close to the scalp (up to 6 inches down the hair shaft in warmer temperatures).
b. They attached to hair by a proteinaceous cement that the female louse secretes.
c. There is NO proven material that can dissolve this cement or facilitating the removal of eggs: This is a business opportunity! Someone should market this cement!
d. Eggs hatch in 7 to 10 days and the immature louse, a nymph begins feeding within 1 minute after hatching
d. The nymph undergoing three molts before reaching the adult stage and achieving reproductive capability within 24 hours after the final molt
4. Here are the treatments available thus far:
A. Lindane (γ-hexachlorocyclohexane): Do NOT USE
b. inhibits the γ-aminobutyric acid (GABA) receptor–chloride channel complex, leading to insect neuronal hyperstimulation, followed by paralysis and death [5].
c. A 1995 systematic review concluded that lindane was insufficiently effective to justify use for head louse infestations [6].
d. It is banned in California:carries a box label warning of serious adverse events, including death, at the recommended dose rate [5, 7, 8]. Lindane is indicated for patients who cannot tolerate or have failed other approved therapies and should be used with caution in infants, children, elderly adults, immunosuppressed individuals, individuals weighing less than 110 pounds, and patients taking seizure medications [8].
B. Pyrethrins and Permethrin (pyrethroids): do NOT use; too much resistance.
b. They are safe but there is a lot of resistance.
C. Malathion (formulated with isopropyl alcohol [78%] and terpineol [12%]): DO NOT USE:
b. Approved by FDA in the 1980s, malathion (0.5%) head louse shampoo but was withdrawn. By 1998, concern about resistance to then-available products led the CDC to request its reinstatement [28].
D. Benzyl Alcohol: I would use this one, though I would likely try the home remedies (though not proven first).
E. Spinosad
b. ok in people 6 months of age and older to treat head lice infestations.
d. Rx needed
e. In two parallel RCTs conducted across the United States, 68.1% of patients in one study and 75.9% in the other were free of lice 14 days after a single spinosad application [18, 19]. Patients who were found to be infested 7 days after one treatment received a second application and were assessed 14 days later. When data from single-application patients were combined with those receiving a second treatment, 84.6% and 86.7% were lice free [18, 34]. Efficacies after a single application without nit combing are strongly suggestive of effectiveness against head lice eggs.
F. Topical Ivermectin 0.5%: I would use this one, though I would likely try the home remedies (though not proven first).
-use FDA approved a 0.5% ivermectin lotion containing olive oil and Shea butter in 2012 for treatment of head lice infestations in patients 6 months of age and older [36]
-2 RCTs conducted across the United States, the effectiveness of 0.5% ivermectin 14 days after a single application, without nit combing, was found to be 76.1% and 71.4% [37].
-it does not have kill eggs directly, but in an ex vivo study, all nymphs died after hatching from ova exposed to the 0.5% lotion for 10 minutes.
-it paralyzes the mouth of the lice: yuck[39].
-there is no data negative skin reactions with this [42].
G. Nonregistered Remedies
Ivermectin Tablets for Oral Administration: I would avoid oral meds in kids.
b. Used in 2 years of age and older in Israel, France, and Ireland, all weighing more than 15 kg, received two treatments with ivermectin tablets (400 μg/kg) 1 week apart [43]. Final assessments 1 week after the second treatment found that lice had been eliminated from 95.2% of subjects. Although this outcome is promising, further data is needed
Dimethicone
b. mechanism of action is not known [44, 45]. No data are available to support the effectiveness or safety of the formulation available in the United States.
Authors say:
Home remedies such as petroleum jelly, olive oil, and mayonnaise have been found to be ineffective ex vivo [2, 46]. These therapies may transiently suppress louse metabolic activity, giving the false impression of death, only to have them awaken shortly thereafter—the so-called “resurrection effect” [31]. Essential oils (such as melaleuca [tea tree] oil), often described as “natural” therapies, have no clinical data to support their use in the United States. Moreover, there are no studies evaluating the safety of any of these remedies, including their potential for contact sensitization and other potentially severe adverse events [47, 48].
I think we need good randomized controlled studies on home remedies such as lemon juice, hydrogen peroxide, Listerine for lice before we say for sure these do not work. Still, it you have a persistent Lice Infestation, go with:
a. 5% benzyl alcohol
b. Topical Ivermectin 0.5%:
Healthtap me if you need an Rx
www.healthtap.com/cremers
Sandra Lora Cremers, MD, FACS
Management of Head Louse Infestations in the United States-A Literature Review.
Abstract
REPORTS:
as benzyl alcohol requires two applications. Home remedies such as mayonnaise, and essential oils, have not been demonstrated to be safe or effective, and may carry potential for severe adverse events. The high risk of failure of over-the-counter treatments in eliminating head louse infestations drives a need for health care provider recognition of the limitations of current treatments and for judicious use of treatme