Can My Child Go to School?
Those of us who have kids have many days when our little ones wake up or even go to bed not feeling their best. Here is help to make those on-the-spot decisions when your little one wakes up on a weekday and is not feeling his best.
1. Your chid woke up with a stomach ache.
What could it be?
The most common cause for stomach ache, especially for children, is pain due to the food that was eaten hours before. Evaluate what your child ate the night before and see if excess sugar and carbohydrates and fatty foods can be the cause. Be sure your chid did not get into the medicine cabinet as some accidentally ingested drugs need to be pumped out of the stomach.
What should you do?
Check your child’s temperature. A child’s normal temperature is around 98.6°F (37°C) when taken orally (in your child’s mouth) and 99.6°F (37.5°C) when taken rectally (in your child’s bottom), your Many doctors define a fever as an oral temperature above 99.5°F (37.5°C) or a rectal temperature above 100.4°F (38°C).
If your chid does not have a fever, it is most likely not a virus or bacteria and thus not contagious. Be sure to give your child plenty of fluids and avoid fatty foods, dairy, even excessive carbohydrates for the first 24 hours. This will help your child process the food that was causing the symptoms better. Stick with the BRAT diet: Bananas, Rice, Apple Sauce, and Toast. For ages, these have been felt to be the least stimulating foods to the stomach in such situations. Toast does have gluten, so avoid if your chid is gluten free. I will look to see if there are any scientific studies on the BRAT diet.
Are stomach aches contagious?
Stomach aches alone are not contagious. A child who has a fever is considered to be contagious. A child who is vomiting with a fever can contaminate a child who is exposed directly to the sick child’s secretions: either by touching the same toys, door knobs that child had touched, touching or inhaling the sick child’s secretions.
Stomach aches alone are not contagious. A child who has a fever is considered to be contagious. A child who is vomiting with a fever can contaminate a child who is exposed directly to the sick child’s secretions: either by touching the same toys, door knobs that child had touched, touching or inhaling the sick child’s secretions.
Send her to school? If your child is fever free, drinking and eating adequately, energetic, and only mildly bothered by her stomach, she doesn’t need to stay at home unless her symptoms persist or get worse.
Keep her home: If there is any fever or she is not able to stand, walk, or play. If there is severe vomiting and she cannot keep anything down or has a persistent high fever (depending on her general health: children who are immunocompromised should see their MD at any sign of stomach ache even without a fever) see your pediatrician. If the stomach pain is intolerable, has severe vomiting with or without a fever, go to urgent care or ER: it could be appendicitis and needs immediate evaluation to before rupture of the appendix.
2. Your child woke up in the middle of the night screaming that her ear hurt. You settled her back to sleep and in the morning she says it feels better.
What could it be?
Ear infection (acute otitis media). This is common during a cold or in swimmers (known as swimmer’s ear). Ear infections have an abrupt onset, and may be associated with a fever, nausea, and vomiting. They are typically get worse when the child is lying down, chewing or sucking, and may cause transient hearing difficulties. Ear infections often feel worse at night, but by morning the pain may be gone.
Fluid behind eardrum (serous otitis media) This usually occurs as a result of blockage in the Eustachian tube: the passageway that connects the middle ear to the throat. It causes a popping sound and a sense of fullness in the ear, much like the feeling you get on an airplane.
A child with a sore throat or dental problems can sometimes also complain of ear pain.
What should I do?
Send her to school? A school-aged child with ear pain should see a doctor sometime the same day to determine its cause. In the meantime, she can attend school if she’s feeling reasonably well, has no other health issues and is fever free, is eating and drinking, and her pain is well controlled with acetaminophen or ibuprofen.
Keep her home! If your little one still has an earache after taking pain medication, there’s no sense sending her to school because she won’t be able to concentrate. Take her to the doctor that day.
3. Your child refuses to eat breakfast and cries that she doesn’t want to go to school because her throat hurts.
What could it be?
Be sure there was no trauma to the throat. My surgical colleague noted that his son had a sore throat when he woke up. When they asked the other children what his son was doing that morning. His daughter noted the son had been trying to fit the metal vacuum tube down his throat. Needless to say, that son when to school after a scolding.
If there is not history of throat trauma, infection of the throat, tonsils and surrounding areas is the most common cause of a sore throat.
If your child is sneezing, and has watery eyes, a slight fever, aches or mild headache, her sore throat is likely caused by a virus and will resolve without medication. But if symptoms include a fever, stomach ache, headache, swollen glands and, possibly, a fine red rash, she may have a bacterial infection such as strep throat. Step throat needs evaluation by your pediatrician.
Allergies: Itchy eyes, a scratchy throat and runny nose without a fever are most likely caused by allergies.
What should I do?
Send her to school? If your child is fever free, drinking and eating adequately, energetic and only mildly bothered by her throat, she doesn’t need to stay at home unless her symptoms persist or get worse.
Keep her home! If her glands are swollen, she’s having difficulty swallowing, has a headache or stomach ache and a rash or fever greater than 99.5°F (37.5°C) or a rectal temperature above 100.4°F (38°C), keep her home from school and take her to the doctor that day. A trip to the ER is appropriate if your child can’t swallow or is having difficulty breathing.
4. Your son wakes up and his eyelids are stuck together. He complains that his eyes are itchy, but otherwise says he feels perfectly well.
What could it be?
Eye infection: The most common cause of eyelids stuck together is blepharitis due to common bacteria on our bodies or Demodex mites making their home on the eyelashes. If your child was not sick recently and/or has no itching, blepharitis is the most common cause and can be treated with warm compresses to clean the area, diluted Tea Tree Oil, Cliradex wipes or Avenova spray. See details at: https://drcremers.com/2016/05/how-to-use-tea-tree-oil-for-eyelid.html
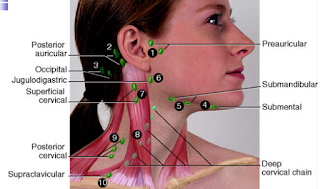
If your child has had a cold or has severe clear discharge and/or itching, a common eye infection is viral conjunctivitis or PINK EYE. This is the “true” Pink Eye which is highly contagious, can cause months of misery due to Epidemic Keratoconjunctivitis (EKC) which can rarely lead to permanent scar tissue on the cornea. Viral conjunctivitis causes the whites of the eyes to appear red and feel itchy and eyelids to sometimes stick together after sleep because of discharge. One or both eyes may be affected. Feel for preauricular lymph nodes: if you feel the, viral conjunctivitis is most likely the diagnosis. If you do not, blepharitis &/or allergic conjunctivitis is most likely.
Allergies: If your child has itchy eyes, a scratchy feeling in his throat and a runny nose with clear mucus, he likely has environmental allergies. His eyes may look bloodshot, but he’s not contagious. Does your child have a history of allergies or has a new pet? If yes, it is likely due to allergy. Allergic conjunctivitis can look just like viral conjunctivitis as the beginning. Feel for preauricular lymph nodes: if you feel the, viral conjunctivitis is most likely the diagnosis. If you do not, blepharitis &/or allergic conjunctivitis is most likely. Allergies If your child has itchy eyes, a scratchy feeling in his throat and a runny nose with clear mucus, he likely has environmental allergies. His eyes may look bloodshot, but he’s not contagious.
Corneal abrasion: A scrape or scratch on the surface of the eye associated with eye pain, tearing and redness.
What should I do?
Send him to school? If your child does not have a cold, does not have a fever, and does not have a rash, your child can go to school as it is likely blepharitis or allergic conjunctivitis.
If your chid has a cold and his eye is red and itchy, see your EyeMD or OD. It can take 2 weeks for viral conjunctivitis to resolve. We now have rapid tests for adenovirus, the most common cause for viral conjunctivitis.
Keep him home & See your doctor if he wakes up with eyelids that are stuck together with a fever and itchy, pink eyes (often associated with ear infections) and/or if there is redness or puffiness of upper or lower eyelids and/or if there is a rash or blister near the eye, or pain is persistent.
5. In the middle of the night, you heard a brassy cough coming from your child’s bedroom. Come morning, his cough has subsided but he’s complaining of a sore throat. He eats a good breakfast and doesn’t have a fever.
What could it be?
Croup A: A viral infection that causes swelling in the upper airway, croup is more common in kids under the age of five. It typically starts with cold symptoms followed by a barking seal-like cough that appears in the middle of the night. It may be accompanied by a low-grade fever, sore throat and loud squeaky noises when your child breathes in. Croup is usually a mild illness, but occasionally causes breathing difficulties. In older kids, croup often presents itself as a hoarse voice (laryngitis).
Common cold: If he’s sneezing and has a runny nose and wet-sounding cough — with or without a low-grade fever — a cold is likely the cause.
What should I do?
Send him to school? If your child has a cold but no fever, he can attend school. Likewise with mild croup, as long as he feels well enough to participate at school and has no difficulty breathing.
Keep him home if cold symptoms worsen after five days or a cough lasts longer than 10, head to the doctor. Go to the ER if symptoms include a high fever, difficulty breathing, severe sore throat, drooling (this implies difficulty swallowing) or rapid breathing.
6. My child ran outside before school and gashed his knee: What should I do?
Dirt and bacteria may cause cuts, scrapes and wounds to become infected. Once the bleeding stops, remove any foreign particles and wash the area with mild soap and tap water. Once the area is clean (clean with warm water & mild soap; apply Betadine or gently bot area with alcohol if you do not have Betadine: but warn child it will burn & blow on area to help with area (your breath will not infect the wound), apply an antibiotic ointment, such as Polysporin, and cover it with a bandage.
See a doctor if:
• the cut is deep or gaping, or edges are separated
• your child has a gaping cut on her face
• dirt can’t be removed
• bleeding does not stop within several minutes after pressure has been applied
• it’s a puncture wound
• your child has a gaping cut on her face
• dirt can’t be removed
• bleeding does not stop within several minutes after pressure has been applied
• it’s a puncture wound
Red alert:
If your child has a deep or dirty cut, such as a wound caused by stepping on a nail or an animal bite, a tetanus needle may be required if her immunizations are not up to date.
Bumps and bruises
Injuries to soft tissues produce pain, swelling and discoloration. If your little guy continues his activities without showing signs of pain, the injury is most likely mild and doesn’t require medical treatment. However, if he has severe pain, swelling or deformity, or avoids using the injured body part, a trip to the doctor is warranted.