Causes of Jaundice
A HealthTap patient asked: Eyes and skin yellow, mass on upper right side and middle abdomen, fever, vomiting, black moles on arms face shoulders v, back, stomach, green to dark. What is causing this.
Answer:
Yellow eyes & skin indicate jaundice which is due to many reasons: hepatitis, liver issues.
The below are excellent reviews that will help pinpoint the cause.
Sandra Lora Cremers, MD, FACS
Jaundice in Adults
In jaundice, the skin and whites of the eyes look yellow. Jaundice occurs when there is too much bilirubin (a yellow pigment) in the blood—a condition called hyperbilirubinemia.
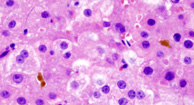
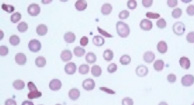
Bilirubin is formed when hemoglobin (the part of red blood cells that carries oxygen) is broken down as part of the normal process of recycling old or damaged red blood cells. Bilirubin is carried in the bloodstream to the liver, where it binds with bile. Bilirubin is then moved through the bile ducts into the digestive tract, so that it can be eliminated from the body. Most bilirubin is eliminated in stool, but a small amount is eliminated in urine. If bilirubin cannot be moved through the liver and bile ducts quickly enough, it builds up in the blood and is deposited in the skin. The result is jaundice.
Many people with jaundice also have dark urine and light-colored stool. These changes occur when a blockage or other problem prevents bilirubin from being eliminated in stool, causing more bilirubin to be eliminated in urine.
If bilirubin levels are high, substances formed when bile is broken down may accumulate, causing itching all over the body. But jaundice itself causes few other symptoms in adults. However, in newborns with jaundice high bilirubin levels (hyperbilirubinemia) can cause a form of brain damage called kernicterus. Also, many disorders that cause jaundice cause other symptoms or serious problems. These symptoms may include nausea, vomiting and abdominal pain, and small spiderlike blood vessels that are visible in the skin (spider angiomas). Men may have enlarged breasts, shrunken testes, and pubic hair that grows as it does in women.
Serious problems can include
-
Ascites: Accumulation of fluid within the abdomen
-
Coagulopathy: A tendency to bleed or bruise
-
Hepatic encephalopathy: Deterioration of brain function because the liver malfunctions, allowing toxic substances to build up in the blood, reach the brain, and cause changes in mental function (such as confusion and drowsiness)
-
Portal hypertension: High blood pressure in the veins that bring blood to the liver, which can lead to bleeding in the esophagus and sometimes stomach
If people eat large amounts of food rich in beta-carotene (such as carrots, squash, and some melons), their skin may look slightly yellow, but their eyes do not turn yellow. This condition is not jaundice and is unrelated to liver disease.
Causes of Jaundice
Jaundice has many causes. Most causes involve disorders and drugs that
View of the Liver and Gallbladder
The most common causes of jaundice are
-
A toxic reaction to a drug or medicinal herb
Hepatitis
Hepatitis damages the liver, making it less able to move bilirubin into the bile ducts. Hepatitis may be acute (short-lived) or chronic (lasting at least 6 months). It is usually caused by a virus. Acute viral hepatitis is a common cause of jaundice, particularly jaundice that occurs in young and otherwise healthy people. Sometimes hepatitis is caused by an autoimmune disorder or use of certain drugs. When hepatitis is caused by an autoimmune disorder or a drug, it cannot be spread from person to person.
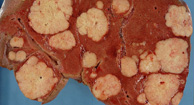
Alcoholic liver disease
Drinking large amounts of alcohol over a long period of time damages the liver. The amount of alcohol and time required to cause damage varies, but typically, people must drink heavily for at least 8 to 10 years. Other drugs, toxins, and some herbal products can also damage the liver (see Table: Some Causes and Features of Jaundice).
Bile duct obstruction
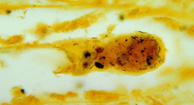
If the bile ducts are blocked, bilirubin can build up in the blood. Most blockages are caused by a gallstone, but some are caused by cancer (such as cancer in the pancreas or bile ducts) or rare liver disorders (such as primary biliary cholangitis or primary sclerosing cholangitis).
Other causes of jaundice
Less common causes of jaundice include hereditary disorders that interfere with how the body processes bilirubin. They include Gilbert syndrome and other, less common disorders such as Dubin-Johnson syndrome. In Gilbert syndrome, bilirubin levels are slightly increased but usually not enough to cause jaundice. This disorder is most often detected during routine screening tests in young adults. It causes no other symptoms and no problems.
Evaluation of Jaundice
Jaundice is obvious, but identifying its cause requires a doctor’s examination, blood tests, and sometimes other tests.
Warning signs
In people with jaundice, the following symptoms are cause for concern:
-
Severe abdominal pain and tenderness
-
Changes in mental function, such as drowsiness, agitation, or confusion
-
Blood in stool or tarry black stool
-
Blood in vomit
-
Fever
-
A tendency to bruise or to bleed easily, sometimes resulting in a reddish purple rash of tiny dots or larger splotches (which indicate bleeding in the skin)
When to see a doctor
What the doctor does
Doctors first ask questions about the person’s symptoms and medical history. Doctors then do a physical examination. What they find during the history and physical examination often suggests a cause and the tests that may need to be done (see Table: Some Causes and Features of Jaundice).
Doctors ask when the jaundice started and how long it has been present. They also ask when urine started to look dark (which usually occurs before jaundice develops). People are asked about other symptoms, such as itching, fatigue, changes in stool, and abdominal pain. Doctors are particularly interested in symptoms that suggest a serious cause. For example, sudden loss of appetite, nausea, vomiting, pain in the abdomen, and fever suggest hepatitis, particularly in young people and people with risk factors for hepatitis. Fever and severe, constant pain in the upper right part of the abdomen suggest acute cholangitis (infection of the bile ducts), usually in people with a blockage in a bile duct. Acute cholangitis is considered a medical emergency.
Doctors ask people whether they have had liver disorders, whether they have had surgery that involved the bile ducts, and whether they take any drugs that can cause jaundice (including alcohol, over-the-counter drugs, medicinal herbs, and other herbal products such as teas). Knowing whether family members have also had jaundice or other liver disorders can help doctors identify hereditary liver disorders.
Because hepatitis is a common cause, doctors ask particularly about conditions that increase the risk of hepatitis, such as
-
Working at a day care center
-
Living in or working at an institution with long-term residents, such as a mental health care facility, prison, or long-term care facility
-
Living in or traveling to an area where hepatitis is widespread
-
Participating in anal sex
-
Eating raw shellfish
-
Injecting illegal or recreational drugs
-
Having hemodialysis
-
Sharing razor blades or toothbrushes
-
Getting a tattoo or body piercing
-
Working in a health care facility without being vaccinated against hepatitis
-
Having had a blood transfusion before 1992
-
Having sex with someone who has hepatitis
-
Having been born between 1945 and 1965
During the physical examination, doctors look for signs of serious disorders (such as fever, very low blood pressure, and a rapid heart rate) and for signs that liver function is greatly impaired (such as easy bruising, a rash of tiny dots or splotches, or changes in mental function). They gently press on the abdomen to check for lumps, tenderness, swelling, and other abnormalities, such as an enlarged liver or spleen.
Testing
Tests include the following:
Liver function tests (also called liver enzyme tests) involve measuring blood levels of enzymes and other substances produced by the liver. These tests help doctors determine whether the cause is liver malfunction or a blocked bile duct. If a bile duct is blocked, imaging tests, such as ultrasonography, are usually required.
Other blood tests are done based on the disorder doctors suspect and the results of the examination and the initial tests. They may include
-
Tests to assess the blood’s ability to clot (prothrombin time and partial thromboplastin time)
-
Tests to check for hepatitis viruses or abnormal antibodies (due to autoimmune disorders)
-
A complete blood count
-
Blood cultures to check for infection of the bloodstream
-
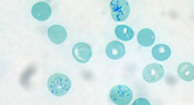
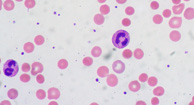
Examination of a blood sample under a microscope to check for excessive destruction of red blood cells
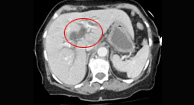
If imaging is needed, ultrasonography of the abdomen is often done first. It can usually detect blockages in the bile ducts. Alternatively, computed tomography (CT) or magnetic resonance imaging (MRI) may be done.
If ultrasonography shows a blockage in a bile duct, other tests may be needed to determine the cause. Typically, magnetic resonance cholangiopancreatography (MRCP) or endoscopic retrograde cholangiopancreatography (ERCP) is used. MRCP is MRI of the bile and pancreatic ducts, done with specialized techniques that make the fluid in the ducts appear bright and the surrounding tissues appear dark. Thus, MRCP provides better images of the ducts than conventional MRI. For ERCP, a flexible viewing tube (endoscope) is inserted through the mouth and into the small intestine, and a radiopaque contrast agent is injected through the tube into the bile and pancreatic ducts. Then x-rays are taken. When available, MRCP is usually preferred because it is just as accurate and is safer. But ERCP may be used because it enables doctors to take a biopsy sample, remove a gallstone, or do other procedures.
Occasionally, liver biopsy is needed. It may be done when certain causes (such as viral hepatitis, use of a drug, or exposure to a toxin) are suspected or when the diagnosis is unclear after doctors have the results of other tests.
Laparoscopy may be done when other tests have not identified why bile flow is blocked. For this procedure, doctors make a small incision just below the navel and insert a viewing tube (laparoscope) to examine the liver and gallbladder directly. Rarely, a larger incision is needed (a procedure called laparotomy).
Treatment of Jaundice
The underlying disorder and any problems it causes are treated as needed. If jaundice is due to acute viral hepatitis, it may disappear gradually, without treatment, as the condition of the liver improves. However, hepatitis may become chronic, even if the jaundice disappears. Jaundice itself requires no treatment in adults (unlike in newborns—see Jaundice in Newborns).
Usually, itching gradually disappears as the liver’s condition improves. If itching is bothersome, taking cholestyramine by mouth may help. However, cholestyramine is ineffective when a bile duct is completely blocked.
If the cause is a blocked bile duct, a procedure may be done to open the bile duct. This procedure can usually be done during ERCP, using instruments threaded through the endoscope.
Essentials for Older People: Jaundice
In older people, the disorder causing jaundice may not cause the same symptoms as it typically does in younger people, or the symptoms may be milder or harder to recognize. For example, if older people have acute viral hepatitis, they often have much less abdominal pain than younger people. When older people become confused, doctors may mistakenly diagnose dementia and not realize that the cause is hepatic encephalopathy. That is, doctors may not realize that brain function is deteriorating because the liver is unable to remove toxic substances from the blood (as it usually does) and, thus, the toxic substances can reach the brain.
In older people, jaundice usually results from a blockage in the bile ducts, and the blockage is more likely to be cancer. Doctors suspect that the blockage is cancer when older people have lost weight, have only mild itching, have no abdominal pain, and have a lump in the abdomen.
Key Points
-
If damage to the liver is severe, jaundice may be accompanied by serious problems, such as deterioration of brain function and a tendency to bleed or bruise.
-
Acute viral hepatitis is a common cause of jaundice, particularly in young and otherwise healthy people.
-
People should see a doctor promptly if they have jaundice so that the doctor can check for serious causes.
-
Cholestyramine may help relieve itching.
Symptoms of jaundice
If an underlying health condition such as viral hepatitis is to blame for the jaundice, you might experience other symptoms, such as excessive fatigue and vomiting.Yellow-tinted skin and eyes characterize jaundice. In more severe cases, the whites of your eyes may turn brown or orange-colored. You may also have dark urine and pale stools.
Some people misdiagnose themselves when they experience yellow skin. According to the Merck Manual, patients who have jaundice usually have both yellow-colored skin and yellow-colored eyes. If you only have yellow skin, it’s maybe due to having too much beta carotene in your system. Beta carotene is an antioxidant found in foods such as carrots, pumpkins, and sweet potatoes. An excess of this antioxidant is not a cause of jaundice.
Causes of jaundice
Your liver might be damaged and unable to perform this process. Sometimes, the bilirubin simply can’t make it to your digestive tract, where it normally would be removed through your stool. In other cases, there may be too much bilirubin trying to enter the liver at once, or too many red blood cells dying at one time.Old red blood cells travel to your liver, where they’re broken down. Bilirubin is the yellow pigment formed by the breakdown of these old cells. Jaundice occurs when your liver doesn’t metabolize bilirubin the way it’s supposed to.
Jaundice in adults is often indicative of:
Jaundice is also a frequent occurrence in newborns, especially in babies who are born prematurely. An excess of bilirubin may develop in newborns because their livers haven’t fully developed yet.
Tests and diagnosis
Other diagnostic tests may be used, including:Your doctor will first conduct blood tests to determine the cause of your jaundice. A blood test can not only determine the total amount of bilirubin in your body, but it can also help detect indicators of other diseases such as hepatitis.
The severity of jaundice in newborns is generally diagnosed with a blood test. A small blood sample is taken by pricking the infant’s toe. Your pediatrician will recommend treatment if the results indicate moderate to severe jaundice.
Treating jaundice
According to the American Liver Foundation, most jaundice cases in infants resolve within one to two weeks.Again, jaundice itself is not a disease but it’s a symptom of several possible underlying illnesses. The type of treatment your doctor recommends for jaundice depends on the cause of your jaundice. Your doctor will treat the cause of the jaundice, not the symptom itself. Once treatment begins, your yellow skin will likely return to its normal state.
Moderate jaundice is typically treated with phototherapy in the hospital or in the home to help remove excess bilirubin.
The light waves used in phototherapy are absorbed by your baby’s skin and blood. The light helps your baby’s body change the bilirubin into waste products to be eliminated. Frequent bowel movements with greenish stools are a common side effect of this therapy. This is just the bilirubin exiting the body. Phototherapy may involve the use of a lighted pad, which mimics natural sunlight and is placed on your baby’s skin.
Severe cases of jaundice are treated with blood transfusions to remove bilirubin.
Outlook for jaundice
Jaundice usually clears up when the underlying cause is treated. Outlook depends on your overall condition. See your doctor right away as jaundice may be a sign of a serious illness. Mild cases of jaundice in newborns tend to go away on their own without treatment, and cause no lasting liver issues.
Email