Conjunctivochalasis:
Conjunctivochalasis is a common condition in which there are extra folds of the conjunctiva, the clear covering over the sclera (the white part of the eye). CCH can cause chronic eye pain, irritation, foreign body sensation, redness, tearing, burning. If conservative treatments do not help (lid hygiene with warm compresses, artificial tears, increased Omega 3 intake, Doxycycline pills, Restasis, etc), we recommend a laser to try to tack back down the conjunctiva to the sclera. If this does not help, then we excise the extra, redundant conjunctiva with a surgical excision and replacement with amniotic membrane (obtained in a sterile condition and tested for safety from a placenta of a newborn baby from FDA approved companies who have obtained these placentas from mothers who have given their consent).
More information below from a great site:
http://webeye.ophth.uiowa.edu/eyeforum/cases/162-conjunctivochalasis.htm
February 6, 2013
Chief Complaint: Watery, irritated eyes
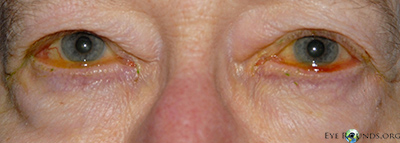
History of Present Illness: This patient was a
healthy 76-year-old woman with complaints of irritated, red, and watery
eyes. She had been followed in our clinic for these concerns and was
being managed with doxycycline 100 mg daily, Lotemax® (loteprednol
etabonate ophthalmic suspension) daily to both eyes, artificial tears,
and artificial tear ointment to both eyes. She felt this regimen had
helped relieve some of her symptoms, but was still bothered by ocular
irritation, intermittent epiphora, and blurriness of her vision while
reading.
Examination:
Visual Acuity with Correction:
- Right eye (OD): 20/20
- Left eye (OS): 20/20-3
Intraocular Pressure (mm Hg)
- OD: 14
- OS: 15
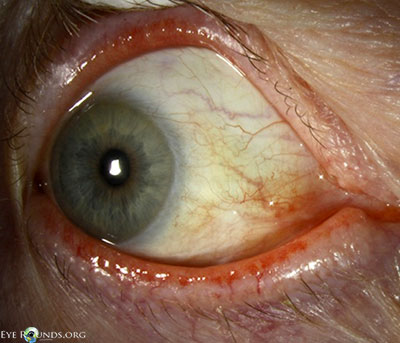
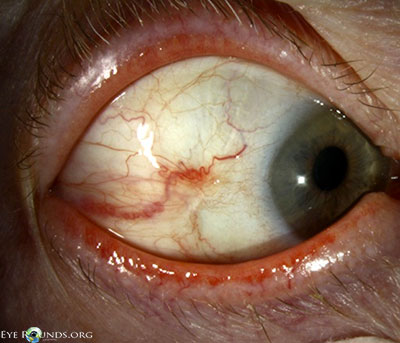
Slitlamp Examination:
- External examination: Conjunctivochalasis apparent on gross examination
- Lids: dermatochalasis, meibomian gland dysfunction, no lagophthalmos, both eyes (OU)
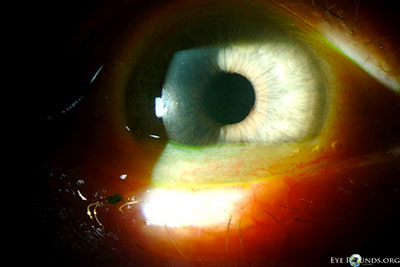
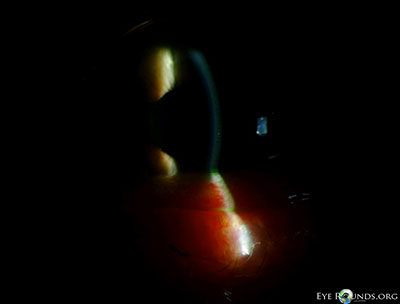
- Anterior segment: marked conjunctivochalasis, corneas clear
without punctate epithelial erosions, anterior chamber deep and quiet,
normal iris architecture, 1-2+ nuclear sclerosis - Posterior segment: within normal limits OU
 |
 |
 |
 |
 |
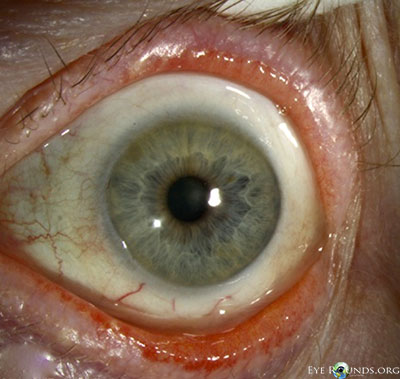
Given her symptoms and failure to respond to medical management as
well as the marked conjunctivochalasis, the patient elected to proceed
with surgery. The operative plan included resection of the excessive
inferior and nasal bulbar conjunctiva with placement of an amniotic
membrane graft. She underwent the procedure first on her right eye and
noted a great amount of improvement in her symptoms, especially the
blurriness while reading. The same operative procedure was performed
four months later in her left eye. She was followed for over one year
after surgery on her right eye (and over six months postoperatively on
her left eye) and continued to be symptomatically improved compared to
preoperatively.
Video: Conjunctival resection with placement of AMT (amniotic membrane transplant)
Conjunctival resection with amniotic membrane graft for conjunctivochalasis
If video fails to load, see http://vimeo.com/59018451
 |
 |
 |
 |
 |
 |
Discussion:
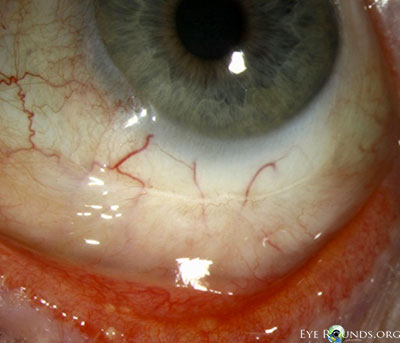
Conjunctivochalasis (CCh) is defined as redundant conjunctiva. Hughes
first coined this entity in 1942; [1] however the description of loose,
nonedematous conjunctiva had been first reported as early as 1908 by
Elschnig.[2] It is most often evident between the globe and the lower
eyelid, but in more advanced cases can be evident around the entire
globe. The majority of cases are bilateral, and often
conjunctivochalasis is overlooked as a normal variant associated with
the aging process if the patient is asymptomatic. In cases where the
patient is symptomatic, common symptoms include: tearing, foreign body
sensation, ocular irritation, and blurriness, especially in down gaze.
It is important to keep this condition in the differential of chronic
ocular irritation and epiphora.
Conjunctivochalasis is a common finding among older adults. Studies
suggest that conjunctivochalasis is more common in patients who have dry
eye and meibomian gland disease/blepharitis and is associated with
contact lens wear.[3] The etiology of conjunctivochalasis is not well
understood. Theories include that it could be a natural aging process of
the conjunctiva or that it could be due to lid position abnormalities,
ocular movements, ocular irritation, and eye rubbing. Some
histopathologic studies demonstrate elastosis, chronic, nongranulomatous
inflammation, fragmentation of the elastic fibers, and loss of
collagen. Matrix metalloproteinases (MMPs) are enzymes that modify or
degrade the extracellular matrix. MMP-1 and MMP-3 enzymes have been
noted to be overexpressed in conjunctivochalasis fibroblasts in tissue
culture, while the enzyme levels of tissue inhibitors of
metalloproteinases (TIMPs) are unchanged. The change in the balance
between these two groups of enzymes may facilitate the breakdown of the
extracellular changes and lead to the clinically evident changes
observed in conjunctivochalasis.[4] Another hypothesis is that pressure
from the eyelids may lead to impaired lymphatic drainage of the
conjunctiva, which is supported by findings of lymphangiectasia,
fragmentation of the elastic fibers, and no signs of inflammation on
histopathology.[5]
If the patient has conjunctivochalasis but is asymptomatic, no
treatment is necessary. For symptomatic patients, medical treatment is
recommended as the initial step. Medical management includes the use of
ocular lubricants, antihistamines (if there is a component of allergic
conjunctivitis), and topical steroids. In cases where medical management
is insufficient in improving the patient’s symptoms, surgical
intervention may be necessary. Surgical management is directed at
resecting the redundant conjunctival tissue. Several methods have been
described in the literature. The most common methods of surgical
intervention include a crescent-shaped conjunctival resection with or
without sutures, resection with placement of an amniotic membrane graft
(with either sutures or fibrin tissue glue or both), or suture fixation
of the redundant conjunctiva to the globe (without resection). During
procedures where the conjunctiva is resected, a crescent of tissue can
be marked, excised, and left to heal or closed with absorbable suture.
Another method of resection is to make a limbal peritomy, extend
posteriorly with relaxing incisions, and then pull the conjunctiva
anteriorly, resecting the excess tissue that extends past the limbus.[6]
The conjunctiva is then re-approximated near the limbus. Lastly,
amniotic membrane grafting is an option. Once the area of conjunctiva is
excised, an amniotic membrane graft is secured to the globe
corresponding to the excised conjunctival defect, secured with fibrin
tissue glue or absorbable suture, or a combination of the two.[7,8]
Success rates of the various methods appear to be similar. Moderate
to high rates of improvement in symptoms have been reported. In a study
by Yokoi and colleagues, an improvement of symptoms was found in 88.2%
of patients that underwent resection of symptomatic
conjunctivochalasis.[6] Similar success rates were reported by Tseng and
colleagues.[8]
| Grade | Number of folds and relationship to the tear meniscus height |
|---|---|
| 1 | No persistent fold |
| 2 | Single, small fold |
| 3 | More than two folds and not higher than the tear meniscus |
| 4 | Multiple folds and higher than the tear meniscus |
Diagnosis: conjunctivochalasis
Epidemiology
|
Signs
|
Symptoms
|
Treatment
|
Differential Diagnosis:
- Chemosis
- Conjunctival infection or inflammation
- Entropion
- Meibomian gland disease
References:
- Hughes WL. Conjunctivochalasis. Am J Ophthalmology 1942;25:48-51.
- Elschnig A. Beitrag zur Aethiologie und Therapie der cronischen Konjunctivitis. Dtsch Med Wochenschr 1908; 26: 1133-1155.
- Mimura T, Yamagami S, Usui T, et al. Changes of
conjunctivochalasis with age in a hospital-based study. Am J
Ophthalmology. 2009;147:171-177. - Li DQ, Meller D, Liu Y, Tseng SC. Overexpression of MMP-1 and
MMP-3 by cultured conjunctivochalasis fibroblasts. Invest Ophthalmol Vis
Sci. 2000;41:404-410. - Wattanabe A, Yokoi N, Kinoshita S, et al. Clinicopathologic study of conjunctivochalasis. Cornea. 2004;23:294-298.
- Yokoi N, Komuro A, Nishii M, et al. Clinical impact of conjunctivochalasis on the ocular surface. Cornea. 2005;24:524-531.
- Serrano F, Mora LM. Conjunctivochalasis: a surgical technique. Ophthalmic Surgery. 1989;20:883-884.
- Meller D, Maskin SL, Pires RT, Tseng SC. Amniotic membrane
transplantation for symptomatic conjunctivochalasis refractory to
medical treatments. Cornea. 2000;19:796-803. - Meller D, Tseng SC. Conjunctivochalasis: literature review and
possible pathophysiology. Survey of Ophthalmology. 1998; 43: 225-232.
Conjunctivochalasis. Eyerounds.org. February 6, 2013; Available from:
http://www.EyeRounds.org/cases/162-conjunctivochalasis.htm

