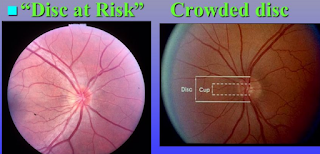
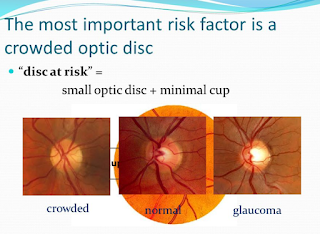
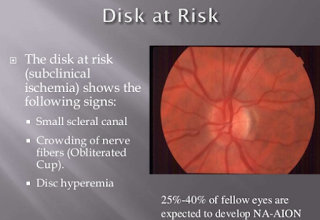
DISC AT RISK:
The normal Cup to Disc Ratio is 0.3
A Disc at Risk has a Cup to Disc Ratio less than 0.3 (usually 0.1).
The optic disc is the region in which the optic nerve attaches to the back of the eye, and the optic cup is a smaller circular region within the disc. The optic nerve fibres that make up the cup allow the central retinal artery and vein to pass through the optic disc to supply blood to the retina and are supplied themselves by very small branching vessels from the posterior ciliary arteries. If the optic nerve fibres are crowded by a small scleral channel, then an ischemic event in the small vessels that supply the optic nerve increases the risk of NAION (Non-Arteritic Ischemic Optic Neuropathy: basically the blood flow to the optic nerve is constricted and causes a loss of oxygen to the retina and optic nerve which leads to a loss of vision: sometimes permanently).
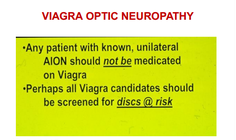
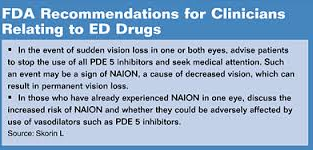
Patients who have a ‘disc at risk’ or ‘crowded disc’ (small cup to disc ratio) are at increased risk for developing NAION. The risk is small. But the risk is increased if a patient smokes, takes hormones (like Oral Contraceptives), or takes erectile dysfunction drugs like PDE 5 inhibitors, vasodilators (ie, Viagra).
In addition to a crowded disc, other established risk factors for NAION include age greater than 50 years and white race (an estimated 95% of cases occur in the latter group). Hypertension and diabetes also predispose to NAION development. Other factors that have been hypothesised to associate with NAION include high cholesterol, arteriosclerosis, stroke, cardiac and intraocular surgery, tobacco use, nocturnal hypotension, blood loss, glaucoma, elevated homocysteine and sleep apnea. The association between NAION and hypertension, high cholesterol and diabetes is stronger in individuals younger than 50 years than in older persons.
If a patient has a disc at risk, I try to gently tell them of this fact without scaring them as the risk overall of having an event like NAION that causes loss of vision permanently is rare (less than 3 patients per 100,000) but since I have seen now 5 patients loss vision permanently from Viagra and many others from Oral Contraceptives (over 10 in my lifetime), I feel the professional and moral obligation to discuss this with patients.
What I tell my patients is that the risk of a problem is low, but patients who have lost vision from an NAION who were on Oral Contraceptives, hormones, or Viagra (PDE5 inhibitors) tended to have disc at risks (either a history of or had it in the other normal eye).
Thus if I have a patient with disc at risks, I tell the patient:
1. Avoid smoking
2. Avoid hormones if at all possible
3. Avoid Viagra and vasodilators
4. Eat healthy diet
5. Any vision darkening or changes in vision, let me know
6. Don’t worry about it otherwise and pray and meditate to keep blood pressure and heart rate always normal
7. If you ever develop high blood pressure, you are the type of patient that SHOULD take a baby aspirin every week or day as recommended by your cardiologist or internist.
Sandra Lora Cremers, MD, FACS
References:
1. Am J Ophthalmol. 1970 May;69(5):874-6.
Visual loss associated with oral contraceptives.
Smith MS, Kreiger A.
Abstract
PIP:
2. Oral Contraceptives Linked to Glaucoma
NEW ORLEANS — Taking oral contraceptives for more than 3 years doubles a woman’s risk for glaucoma, according to a large population-based study.
“This study is the first to document this risk, and it’s important for the general population,” said lead investigator Ye Elaine Wang, MD, from the University of California at San Francisco. “Postmenopausal women should be reassured that the study does not prove causative effects, but women who have used oral contraceptives for 3 years or more and who have additional risk factors for glaucoma should be checked annually for the disease during their eye exams.”
Dr. Wang presented the findings here at the American Academy of Ophthalmology 2013 Annual Meeting.
Known risk factors for glaucoma include age, race, family history of glaucoma, elevated intraocular pressure, and existing visual field defects.
The cross-sectional study was based on 3406 women 40 years or older who participated in the National Health and Nutrition Examination Survey (NHANES). The participants completed vision and reproductive health questionnaires and underwent eye exams.
The primary outcome measure was self-reported glaucoma, which was not confirmed by any diagnosis, Dr. Wang told Medscape Medical News.
A multivariate analysis, adjusted for confounding factors, found that the use of oral contraceptives for 3 years or more was associated with twice the risk for self-reported glaucoma. These results were consistent regardless of what type of contraceptive the women had used, said Dr. Wang.
Double the Risk
The women were assessed for visual field defects using frequency-doubling technology. Visual field defects in 1 or both eyes was associated with the increased prevalence of glaucoma, but this association was not significant.
Previous studies have suggested that estrogen is implicated in the pathogenesis of glaucoma.
“The current study should be an impetus for future research to look at cause and effect of oral contraceptive use and glaucoma,” said Dr. Wang.
Her team plans to conduct new studies on the relation between oral contraceptive use, visual field defects, elevated intraocular pressure, and abnormal cup-to-disk ratio in the optic nerve.
This study did not show that these women actually had the diagnosis of glaucoma, said Darrell WuDunn, MD, from the Eugene and Marilyn Glick Eye Institute at the Indiana University School of Medicine in Indianapolis.
Anyone older than 40 should be screened for glaucoma and have their eyes examined by an ophthalmologist.
Dr. WuDunn said it would be important to know participants’ level of medical knowledge, and whether they were more or less likely to see a physician, but these questions were not included in the survey.
“The hypothesis is that estrogen therapy plays a protective role against glaucoma. Postmenopausal women have an increased risk for glaucoma, compared with men of similar age. Oral contraceptives suppress the peak and trough levels of estrogen and maintain a consistent level. This could explain the increased risk for glaucoma, but the study doesn’t show that,” he noted.
Dr. WuDunn said that it is too early to make recommendations about contraceptive use and risk for glaucoma, but he added that “anyone older than 40 should be screened for glaucoma and have their eyes examined by an ophthalmologist.”
Dr. Wang reports financial relationships with the National Eye Institute Core Grant, Vision Research Grant, Research to Prevent Blindness That Man May See, and the National Natural Science Foundation of China. Dr. WuDunn has disclosed no relevant financial relationships.
American Academy of Ophthalmology (AAO) 2013 Annual Meeting. Presented November 18, 2013.
Long-term use of the contraceptive pill doubles the risk of a leading cause of blindness, a study has shown.
Scientists warned that the Pill may play a role in glaucoma and urged women at risk to have their eyes screened.
Glaucoma is caused by a build-up of fluid pressure in the eye, resulting in irreversible damage to the optic nerve. The most common, chronic form of the disease is believed to affect about 480,000 people in England.
Previous studies have suggested that the hormone oestrogen, a key component of the Pill, might be involved in the development of glaucoma.
The new finding, presented at the American Academy of Ophthalmology’s annual meeting in New Orleans, follows a study of 3,406 women aged 40 and over who were questioned about their reproductive history and underwent eye examinations.
Researchers found that women who had used oral contraceptives for three years or more were twice as likely to have had a diagnosis of glaucoma.
It made no difference what kind of oral contraceptive the women had been using.
The scientists said taking the Pill long-term could be a risk factor for glaucoma that sits alongside others, including family history of the disease, black African ancestry, short-sightedness, raised pressure in the eye, and diabetes.
They urged gynaecologists and eye specialists to be aware of the risk of glaucoma in women who have been on the Pill for a number of years.
Study leader Professor Shan Lin, from the University of California at San Francisco, said: ”This study should be an impetus for future research to prove the cause and effect of oral contraceptives and glaucoma.
”At this point, women who have taken oral contraceptives for three or more years should be screened for glaucoma and followed closely by an ophthalmologist, especially if they have any other existing risk factors.”
There are four main types of glaucoma, the most common being slow-developing chronic open-angled glaucoma.
Primary angle-closure glaucoma is a rare form that can occur slowly or develop quickly, leading to rapid vision loss in one or both eyes.
Secondary glaucoma is the result of an eye injury or other eye condition, such as inflammation. Developmental, or congenital, glaucoma is another rare version of the disease caused by a birth defect.
Edited by Matthew Sparkes
4.
http://www.mayoclinic.org/drugs-supplements/estrogen-and-progestin-oral-contraceptives-oral-route/side-effects/drg-20069422
http://www.mayoclinic.org/drugs-supplements/estrogen-and-progestin-oral-contraceptives-oral-route/side-effects/drg-20069422
Side Effects
Drug information provided by: Micromedex
Healthy women who do not smoke cigarettes have almost no chance of having a severe side effect from taking oral contraceptives. For most women, more problems occur because of pregnancy than will occur from taking oral contraceptives. But for some women who have special health problems, oral contraceptives can cause some unwanted effects. Some of these unwanted effects include benign (not cancerous) liver tumors, liver cancer, or blood clots or related problems, such as a stroke. Although these effects are very rare, they can be serious enough to cause death. You may want to discuss these effects with your doctor.
Smoking cigarettes during the use of oral contraceptives has been found to greatly increase the chances of these serious side effects occurring. To reduce the risk of serious side effects, do not smoke cigarettes while you are taking oral contraceptives. Cigarette smoking increases the risk of serious cardiovascular side effects from oral contraceptive use. The risk increases with age and with heavy smoking (15 or more cigarettes per day) and is quite marked in women over 35 years of age.
Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
The following side effects may be caused by blood clots. Get emergency help immediately if any of the following side effects occur:
Rare
- Abdominal or stomach pain (sudden, severe, or continuing)
- coughing up blood
- headache (severe or sudden)
- loss of coordination (sudden)
- loss of vision or change in vision (sudden)
- pains in chest, groin, or leg (especially in calf of leg)
- shortness of breath (sudden or unexplained)
- slurring of speech (sudden)
- weakness, numbness, or pain in arm or leg (unexplained)
Check with your doctor as soon as possible if any of the following side effects occur:
More common
- Changes in the uterine bleeding pattern at menses or between menses, such as decreased bleeding at menses, breakthrough bleeding or spotting between periods, prolonged bleeding at menses, complete stopping of menstrual bleeding that occurs over several months in a row, or stopping of menstrual bleeding that only occurs sometimes
Less common
- Headaches or migraines (although headaches may lessen in many users, in others, they may increase in number or become worse)
- increased blood pressure
- vaginal infection with vaginal itching or irritation, or thick, white, or curd-like discharge
For women with diabetes mellitus
- Mild increase of blood sugar—Faintness, nausea, pale skin, or sweating
Rare
- Mental depression
- swelling, pain, or tenderness in upper abdominal area
For women who smoke tobacco
- Pains in stomach, side, or abdomen
- yellow eyes or skin
For women with a history of breast disease
- Lumps in breast
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Abdominal cramping or bloating
- acne (usually less common after first 3 months and may improve if acne already exists)
- breast pain, tenderness, or swelling
- dizziness
- nausea
- swelling of ankles and feet
- unusual tiredness or weakness
- vomiting
Less common
- Brown, blotchy spots on exposed skin
- gain or loss of body or facial hair
- increased or decreased interest in sexual intercourse
- increased sensitivity of skin to sunlight
- weight gain or loss
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.