Patients with Dry Eyes initially may not think “a little dry eye” is a big deal. This is true for the majority of patients. However, if left untreated, many patients can progress to debilitating disease. In a small percentage of patients, though, dry eye can lead to true devastation and disability: having chronic pain with every blink can be very difficult to live with for some patients.
Thus comprehensive testing is very important for any patient with dry eyes and their physician. Testing, though, for Dry Eye has been frustrating for patients and physicians alike. Many dry eye tests have a low sensitivity and specificity.
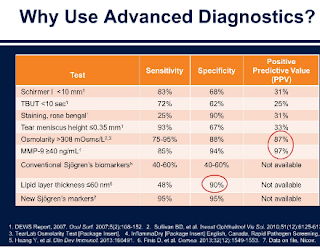
The most classic dry eye tests are noted here and their positive positive test that are true positives (Positive Predictive Value). As you can see the PPV of these classic tests are low.
1. Schirmer: 31%
2. Tear Break Up Time: 25%
3. Staining of Cornea: 31%
4. Tear Meniscus Height 33%
Thus new, innovative ways of diagnosing dry eye or meibomian gland dysfunction have been developed in recent years.
The key issue in many of these tests is that they are expensive and not covered by insurances. Many patients cannot find some of the advanced tests in their doctors offices (especially as many of these tests are not reimbursed by insurances and thus a money loosing issue for offices.) Additionally offices often cannot even charge patients for these tests because of insurance regulations and thus many eyeMD offices are no longer doing many of these tests.
Sandra Lora Cremers, MD, FACS
A. TEAR FILM STABILITY TESTS: A normal tear film should be continuously available from a combination of 3 key areas:
1. Tear Film break-up time (TFBUT or FBUT)
- We use of a microscope called a slit-lamp, set on a bright light setting with a cobalt blue filter
- We Instill fluorescein into the lower fornix.
- Patient blinks several times and then stop.
- We measure the time between the last blink and the first appearance of a dark spot on the cornea (formation of a dry area) on the otherwise continuously stained tear film.
- A tear break-up time of less than 10 seconds suggests a dry eye.
2. Non-invasive tear break up time (NIBUT): no Fluorescein is used & eye is not touched
Fluorescein in the tears may stimulate reflex tearing and may also result in changes to the tear film properties.
1. Schirmer test: there is actually a Schirmer I and Schirmer II test: this describes Schirmer II
- Instil a drop of local anaesthetic into the eye, (optional).
- Prepare a filter paper (5mm x 35mm with folded end).
- Gently dry the eye.
- Apply the filter paper with the folded end hooked onto the lower lid margin at the junction between the middle and outer third (take care not to touch the cornea).
- Tell patient to keep their eye open and blink normally.
- Measure the amount of wetting after 5 minutes: 13-15mm wetting rules out a dry eye; 6-10mm is borderline and less than 6mm indicates dry eye.
- The filter paper strips can cause reflex tearing and may require the use of anaesthetic agents: if not anesthetic agent is used, it measure reflex tearing & is called Schirmer’s I test. These test have fallen out of favor after published reports showed lack of correlation with true dry eye patients.
2. Phenol Red Test
A cotton thread impregnated with phenol red dye is used. Phenol red is pH sensitive and changes from yellow to red when wetted by tears.
- The crimped end of a 70mm long thread is placed in the lower conjunctival fornix.
- After 15 seconds, the length of the colour change on the thread – indicating the length of the thread wetted by the tears -is measured in millimetres.
- Wetting lengths should normally be between 9mm and 20mm. Patients with dry eye have wetting values of less than 9mm.
3. Tear Prism Height Test
A significant amount of information about tear quantity can be gained simply from observing the heights of the upper and lower tear menisci with the slit-lamp biomicroscope.
b. The second technique is to compare the tear prism height with the illuminated slit width by setting the slit horizontally in alignment with the lower lid margin, altering the slit width until it appears to match the height of the tear prism. Heights of less than 0.2mm indicate reduced tear fluid quantity.
c. Observation of the meniscus profile is also extremely helpful. A regular tear meniscus is typically observed in a healthy eye while a meniscus with a scalloped edge is often associated with a dry eye.
1. Rose Bengal Test (No longer widely used)
End-organ damage to conjunctival and corneal epithelial cells can be assessed via Rose Bengal ocular surface staining, which identifies areas of devitalised tissue:
- Instill a drop of Rose Bengal dye into the inferior fornix of the unanesthetised eye.
- Ask the patient to blink twice, to spread the red stain over the conjunctiva and cornea.
- The ideal time to measure the presence of staining is approximately 3 to 5 minutes after instilling the drops.
- Score the staining using a slit-lamp: a pattern of exposure zone (interpalpebral) corneal and bulbar conjunctival staining is typically seen with aqueous tear deficiency.
2. Lissamine Green (less widely used)
Lissamine green staining like Rose Bengal, colours any desiccated and dying cells on the ocular surface. However, lissamine green may be better accepted by patients as it lacks the slight burning or stinging sensation typically found with rose Bengal.
Fluorescein staining penetrates areas of the corneal epithelium and conjunctival epithelium where intercellular junctions are disrupted.
1.
LipiView: exciting new technology but we still do not know what all the data it provides really means in terms of prognosis. It is expensive as well: range $1000-2000 depending if Lipiflow is performed. It available near our office3. SJO: Sjögren’s Test:
Sjögrens is an important diagnosis for eye doctors to NOT miss. All doctors should ask their patients if they have dry mouth and/or arthritis if the patient has any dry eye complaint (like foreign body sensation, rebound tearing, redness).
Sjögrens is a serious diagnosis because of it association with many other issues, in particular, Non-Hodgkin lymphoma which can happen in 5% of people with the syndrome.
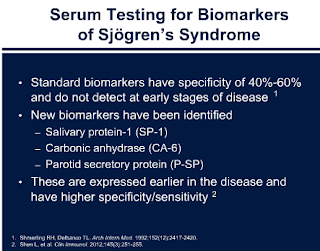
The Sjö test has a Higher Specificity and Sensitivity compared to
40-60% sensitivity of anti-Ro or anti-La (older tests)
Sjo tests include: Salivary Protein-1 (SP-1); Carbonic Anhydrase (CA-6); Parotid Secretory Protein (P-SP)
More information below on Sjogrens:
4. Lipid Analysis: Lipid Layer Thickness <60nm2 is a significant sign that the meibomian glands are not functioning as they should.
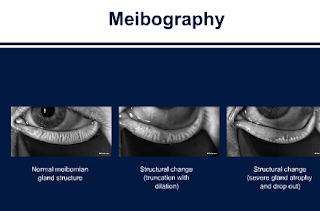
5. Meibography: Shows meibomian glands and their drop out.
It can convince patients they need treatment.
The machine to be able to show patients is still coming to be able to show patients. Harvard and many academic centers do not have this machine yet.
6. Optical Coherence Tomography on the Cornea is starting to be used more and more to assess tear film.
7. Tear Lactoferrin: coming soon: new test
- Modulation of ocular inflammatory response
- Regulation of normal cell growth
- Protection against infections by inhibiting viral, bacterial or fungal growth
———–
http://www.uptodate.com/contents/sjogrens-syndrome-beyond-the-basics
Patient information: Sjögren’s syndrome (Beyond the Basics)
Patient information: Antinuclear antibodies (The Basics)
Patient information: Diffuse large B cell lymphoma in adults (Beyond the Basics)
Patient information: Follicular lymphoma in adults (Beyond the Basics)
Patient information: Fibromyalgia (Beyond the Basics)
Patient information: Vaginal dryness (Beyond the Basics)
Patient information: Allergic rhinitis (seasonal allergies) (Beyond the Basics)
Patient information: Nonallergic rhinitis (runny or stuffy nose) (Beyond the Basics)
Patient information: Acid reflux (gastroesophageal reflux disease) in adults (Beyond the Basics)
Patient information: Nonsteroidal antiinflammatory drugs (NSAIDs) (Beyond the Basics)
Patient information: Disease-modifying antirheumatic drugs (DMARDs) (Beyond the Basics)
Patient information: Insomnia (Beyond the Basics)
Clinical manifestations of Sjögren’s syndrome: Exocrine gland disease
Clinical manifestations of Sjögren’s syndrome: Extraglandular disease
Interstitial lung disease associated with Sjögren’s syndrome: Clinical manifestations, evaluation, and diagnosis
Pathogenesis of Sjögren’s syndrome
Renal disease in Sjögren’s syndrome
Treatment of dry eye in Sjögren’s syndrome
Treatment of dry mouth and other non-ocular sicca symptoms in Sjögren’s syndrome
Treatment of systemic and extraglandular manifestations of Sjögren’s syndrome
(www.ninds.nih.gov/disorders/sjogrens/sjogrens.htm)
(http://www.arthritis.org/conditions-treatments/disease-center/sjoumlgrens-syndrome/)
- Ramos-Casals M, Tzioufas AG, Font J. Primary Sjögren’s syndrome: new clinical and therapeutic concepts. Ann Rheum Dis 2005; 64:347.
- Kassan SS, Moutsopoulos HM. Clinical manifestations and early diagnosis of Sjögren syndrome. Arch Intern Med 2004; 164:1275.
- Fox RI, Stern M, Michelson P. Update in Sjögren syndrome. Curr Opin Rheumatol 2000; 12:391.
- Soto-Rojas AE, Kraus A. The oral side of Sjögren syndrome. Diagnosis and treatment. A review. Arch Med Res 2002; 33:95.
- Ramos-Casals M, Brito-Zerón P, Sisó-Almirall A, et al. Topical and systemic medications for the treatment of primary Sjögren’s syndrome. Nat Rev Rheumatol 2012; 8:399.
- Fox RI. Sjögren’s syndrome. Lancet 2005; 366:321.
- Fox RI, Liu AY. Sjögren’s syndrome in dermatology. Clin Dermatol 2006; 24:393.




 Top
Top