FOOD: How to choose best food to heal your symptoms?
Years ago, it seemed as if no one ever talked about “going Gluten Free,” or “a low inflammatory diet,” or “going Carb Free.”
What is all this craze about?
Mostly, the issue is that traditional medicine does not have all the answers and more research is showing the power of natural foods to heal many patients’ ailments.
Choosing the right foods to heal yourself of a symptoms does not have to be hard.
Following the below simple rules, may help determine the underlying cause of your symptoms or condition, help heal you naturally, and help you and your doctors determine if you DO need traditional medicines which do work for most conditions. Contrary to popular relieve, most MDs, like myself, do prefer to treat patients naturally before trying prescription medicines or surgery.
Genetics plays a big part in one’s health and thus what you choose to eat should be guided by your family and genetic history. For instance, if you have a strong family history of Diabetes, avoid excessive carbohydrates as early in age as possible. If you have a strong family history of prostate cancer, eat plenty of organic tomatoes for the lycopene.
If you are having difficulty recovering from a virus or head cold, focus on increasing your anti-oxidant intake, Vitamin D production, Vitamin C intake ideally naturally & get plenty of fluids and rest: this will help your immune system fight the virus.
If you have chronic headaches and migraines, see my Migraine Diet Sheet to see the best plan of attack (in general): https://drcremers.com/2014/02/migraine-diet-recommended-and-not.html
This
is an area that most MDs are very skeptical about and for good reason:
there have not been great randomized, double blinded controlled studies
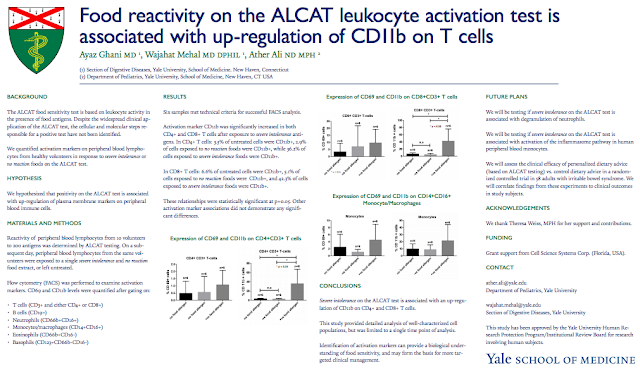
that prove that nature-based diets (such as ALCAT below) works.
However, there has been more research on these tests and diets as noted
below and through links below.
It does make sense: use
certain organic foods to heal yourself. Avoid “dangerous foods.” Try to
rarely eat “potentially dangerous food” based on one’s genetic profile.
Recently
2 MDs friends, one from medical school at Brown, told me of their
journey to be cured of two debilitating disease. Both tried the medical
route: with many prescriptions and side effects.
Finally, after
given up on traditional medicine, they researched alternatives and found
hope if not a total cure in the site below and in natural remedies. One
is still struggling with his diagnosis but feels much better.
I
include the information for patients who want to know more. I have
written about my own unusual diet: currently mostly seaweed, pecans,
almonds, almond milk, Stevia water, and plenty of fresh veggies, salad,
and wild salmon; almost no wheat, rice, and very limited meat: at most
3x/month; eggs about 1-2 per week; cheese & cottage cheese on
occasion; rarely beans (has a lot of fiber but also a lot of carbs). I
do not recommend this diet unless one has a strong family history of
diabetes. But I must note that a few months ago, I started noting a pain
in my left, 2nd finger’s joint (PIP), which for any surgeon is a
concern, soon after the diet change, the pain went away completely. Was
it the humidity, weather, loosing some weight or just the diet change? I
might never know. But my study of 1 was interesting enough to look in
to the below theories.
The next step is for someone to
donate funds to study such theories and diets objectively, without drug
company money. Time will tell if these natural remedies are worth the
out-of-pocket expense they sometime entail.
For now, many MD friends are beginning to look into this to treat themselves and their friends.
I am researching this more to find out what other studies have been done on this particular theory.
Sandra Lora Cremers, MD, FACS
Below
are the sites a close friend from medical school, who was at the top of
her class, used for healing. I am hesitant to endorse these as I have
not used them or been evaluated by ALCAT. However, my friend’s testimony
was so strong, it seems all patients should at least know about these
alternative testing and treatment options especially since few medical
schools discuss these things with med students.
1. https://www.alcat.com/pages/clinical_info/
2.
ALCAT | Available for over 25 years
Alcat Test is a lab based immune stimulation test in which a patient’s
WBC’s are challenged with various substances including foods, additives,
colorings, chemicals, medicinal herbs, functional foods, molds and
pharmaceutical compounds. The patient’s unique set of responses help to
identify substances that may trigger potentially harmful immune system
reactions.

Danuta Mylek studied 72 patients who followed an ALCAT based
elimination diet; they had significant improvement in their symptoms
that included arthritis, bronchitis and gastro issues. Specifically,
they found improvement in 83% of arthritis patients, 75% of Urticaria,
bronchitis, and gastroenteritis patients, 70% of migraine patients, 60% of chronic fatigue syndrome patients,
50% of asthma patients, 49% of AD patients, 47% of rhinitis patients
and 32% of hyperactivity patients. Patients were also skin tested for
IgE allergy to inhalants and foods that were more pronounced in skin and
nasal symptoms. Published in Advances in Medical Sciences; Formerly
Roczniki Akademii Medycznej w Białymstoku Volume 40, Number 3, 1995.
The ALCAT Test – A Guide and Barometer in the Therapy of Environmental and Food Sensitivities
Barbara A. Solomon MD studied 172 patients successfully using an ALCAT
Test-based diet to alleviate the following range of symptoms: classic
migraine (85%), common migraine (62%), sinus headaches (58%),
gastoesphageal reflux (GERD) (75%), IBS (71%), inflammatory arthritis
(65%), recurrent Sinusitis (59%), tension fatigue syndrome (60%), obesity
(50%), eczema (55%), asthma (30%), depression and/or anxiety (31%),
recurrent vaginitis (20%), recurrent urinary tract infection (46%),
degenerative arthritis (44%) and allergic rhinitis (42%). Published in
Environmental Medicine, Volume 9, Number 1 & 2, 1992. Barbara
Solomon MD, MA
Migraine/Headache
Inmunologic de Catalunya. Informe final de resultados estadisticos.
version 3, 28 de diciembre de 2006. (translated English version HERE )
is a study of 21 patients (2 men and 19 women) with migraines and with
positive results on the ALCAT test for at least one evaluated food and
have been included with the objective of comparing the number of
migraines reported during a period of diet of 3 months (phase I) and
another period of 3 months without any dietary restriction (phase II).
The hypothesis of this study began by considering that patients with
migraines have intolerance to certain food, determined by the ALCAT
test. Also, the foods the ALCAT tested as positive aggravated
migraines. Therefore, a diet that avoids these foods would improve
migraines, in the number of monthly attacks, intensity of pain and
duration of the attacks. Study by Immunological Center of Catalunya, IMS
Health: Health Economics and Outcomes Research—Influence of Food
Intolerance in Migraines: Final Report of Statistical Results. Version
3, December 28, 2006.
half of the patients included (47.6%) reduced the number of migraine
attacks per month between the inclusion phase in the study and the phase
of dietary restriction.The percentage of patients that suffered attacks
for more than 12 hours decreased from 57.1% in the inclusion phase to
47.6% in the dietary restriction phase.The frequency of appearance of
accompanying symptoms such as photophobia and phonophobia between the
inclusion phase and the dietary restriction phase was reduced from 47.7%
to 28.4% in the first case and from 35.7% to 23.3% in the second.
Pilot Study Into The Effect of Naturally Occurring Pharmacoactive Agents on the ALCAT Test.
PJ Fell used the ALCAT test to successfully determine cellular
reactions to Pharmacoative agents found in foods that trigger migraine
headaches. Presented at Annual Meeting of the American Otolaryngic
Allergy Association, September 27, 1991; Kansas City, MO. P.J. Fell, MD
ALCAT Test Results In The Treatment of Respiratory and Gastrointestinal Symptoms, Arthritis, Skin and Central Nervous System
Danuta Mylek studied 72 patients who followed an ALCAT based
elimination diet; they had significant improvement in their symptoms
that included arthritis, bronchitis and gastro issues. Specifically,
they found improvement in 83% of arthritis patients, 75% of Urticaria,
bronchitis, and gastroenteritis patients, 70% of migraine patients, 60%
of chronic fatigue syndrome patients, 50% of asthma patients, 49% of AD
patients, 47% of rhinitis patients and 32% of hyperactivity patients.
Patients were also skin tested for IgE allergy to inhalants and foods
that were more pronounced in skin and nasal symptoms. Published in
Advances in Medical Sciences; Formerly Roczniki Akademii Medycznej w
Białymstoku Volume 40, Number 3, 1995.
The ALCAT Test – A Guide and Barometer in the Therapy of Environmental and Food Sensitivities
–Barbara A. Solomon MD studied 172 patients successfully using an ALCAT
Test-based diet to alleviate the following range of symptoms: classic
migraine (85%), common migraine (62%), sinus headaches (58%),
gastoesphageal reflux (GERD) (75%), IBS (71%), inflammatory arthritis
(65%), recurrent Sinusitis (59%), tension fatigue, syndrome (60%),
obesity (50%), eczema (55%), asthma (30%), depression and/or anxiety
(31%), recurrent vaginitis (20%), recurrent urinary tract infection
(46%), degenerative arthritis (44%) and allergic rhinitis (42%).
Published in Environmental Medicine, Volume 9, Number 1 & 2, 1992.
Barbara Solomon MD, MA
PJ Fell PJ, J Brostoff, and MJ Pasula demonstrated in a study of 19
patients an overall correlation between ALCAT and DBC at 83.4%,
suggesting that the ALCAT Test was quite reliable in identifying unsafe
foods in these sensitive subjects. Presented at 45th Annual Congress of
the American College of Allergy and Immunology, Los Angeles, CA:
November 12-16, 1988 Peter I. Fell, MD, Director; Oxford Allergy Centre,
London Jonathon Brostoff, MA DM USc FRCP FRCPath, Dept. of Immunology,
University College & Middlesex School of Medicine, London Mark I.
Pasula, Ph.D., Research Director; AMTL Corp., Miami, F

MORE
THAN ANY other league in American sports, the NBA is an aspirational
technocracy. Adam Silver, its flowchart-savvy new commissioner, travels
the country championing analytics and innovation. The D-League functions
not only as the game’s minor leagues but also, per the NBA’s official
phraseology, as its “research and development laboratory.” And thanks to
the August sale of the Clippers to former Microsoft CEO Steve Ballmer,
about 1 in 3 majority owners in the NBA can now trace their billions to
the tech industry.
So
maybe it shouldn’t be surprising that Silicon Valley is transforming
how teams scrutinize, optimize and fundamentally think about their
players — or that Dr. Leslie Saxon, executive director of the Center
for Body Computing at the University of Southern California, contends
that the NBA is leading society into the biometric revolution. “We’ve
been inundated with all these companies coming up with different things
to look at and test,” says Gregg Farnam, longtime Timberwolves trainer
and the chairman of the National Basketball Athletic Trainers
Association. “It’s the explosion of data and data collection.”
But
what might come as a surprise is how significant that explosion has
been, and how far its blast radius might soon reach. The literary
specter haunting sports’ burgeoning Information Age is no longer Michael
Lewis and Moneyball but George Orwell and 1984.
The
boom officially began during work hours. Before last season, all 30
arenas installed sets of six military-grade cameras, built by a firm
called SportVU, to record the x- and y-coordinates of every person on
the court at a rate of 25 times a second — a technology originally
developed for missile defense in Israel. This past spring, SportVU
partnered with Catapult, an Australian company that produces wearable
GPS trackers that can gauge fatigue levels during physical activity.
Catapult counts a baker’s dozen of NBA clients, including the
exhaustion-conscious Spurs, and claims Mavericks owner Mark Cuban as
both a customer and investor. To front offices, the upside of such
devices is rather obvious: Players, like Formula One cars, are luxury
machines that perform best if vigilantly monitored, regulated and
rested.
But
to follow this logic to its conclusion is to understand why the scope
of this monitoring is expanding, and faster than the public knows. Teams
have always intuited that on-court productivity could be undermined by
off-court choices — how a player exhausts himself after hours, for
instance, or what he eats and drinks. Now the race is on to
comprehensively surveil and quantify that behavior. NBA executives have
discovered how to leverage new, ever-shrinking technologies to supervise
a player’s sleeping habits, record his physical movements, appraise his
diet and test his blood. In automotive terms, the league is investing
in a more accurate odometer.
“We
need to be able to have impact on these players in their private time,”
says Kings general manager Pete D’Alessandro. “It doesn’t have to be us
vs. you. It can be a partnership.”
A
lovely sentiment, at least in theory. But how long will it be until
biometric details impact contract negotiations? How long until graphs of
off-court behavior are leaked to other teams or the press? How long
until employment hinges on embracing technology that some find invasive?
“Employers
dictating the health care of their employees is a conflict of interest
that cannot be overcome,” says Alan C. Milstein, a leading bioethics
attorney and sports litigator who often represents NBA players. “I just
refuse to believe that the purpose of monitoring on any long-term basis
is the health of the employee. If the purpose is to predict performance,
that’s not a health care purpose. That’s an economic purpose.”
No
complaints have been filed to the National Basketball Players
Association as of yet. But it is worth noting that these partnerships
have developed so quietly that the union had not even developed a
position on the concept until ESPN requested comment in August. “If the
league and teams want to discuss potentially invasive testing procedures
that relate to performance, they’re free to start that dialogue and
we’ll be glad to weigh the benefits against the risks,” says longtime
NBPA counsel Ron Klempner, who served as interim executive director from
February 2013 to September 2014. “Obviously, we’d have serious privacy
and other fairness concerns on behalf of the players. We’ve barely left
the starting line on these issues.”
In the meantime, locked doors have swung open already.
ANDRE
IGUODALA’S TV used to cackle into the early morning, the laugh track of
The Fresh Prince of Bel-Air echoing in the semidarkness of his master
bedroom. For years, this was the All-Star swingman’s post-midnight
routine: watch reruns around 2 a.m.; pass out around 4; wake up around
8; drag self to gym; repeat. Iguodala traces the insomnia back to the
University of Arizona, where he’d toss and turn over his pro future. But
it was only last season, with his 30th birthday staring him in the
face, that the newly hired Warrior surrendered his problem to an
employer. “I told them that I needed to see a sleep therapist ASAP,”
Iguodala says. “And it’s funny: Keke told me he’d been thinking about
the same thing.”
Keke
Lyles, Golden State’s director of athletic performance, had already
been researching what amounts to an open secret about NBA slumber:
Players sleep as lightly as undergrads during finals week but nap harder
than Spanish plutocrats. Iguodala’s typical game-day siestas, for
example, ran three to four hours. “Even if they’ve been out all night,”
says Grizzlies trainer Drew Graham, “most of them take naps and think
that’s enough. They see the other guys do it.”
The problem with that strategy, however, is quantifiable.
A Stanford School of Medicine study of 11 men’s basketball players,
published in the journal Sleep in 2011, found that getting 10 hours a
night not only reduced fatigue and injury risk but also improved
accuracy at the foul line (by 9 percent) and behind the arc (9.2
percent). More recently, at the Sloan Sports Analytics Conference in
March, front office execs heard a Harvard Medical School professor
declare that a 25-year-old who sleeps four hours a night for one week
possesses the degraded testosterone levels of someone who’s 36. “If you
told an athlete you had a treatment that would reduce the chemicals
associated with stress, that would naturally increase human growth
hormone, that enhances recovery rate, that improves performance, they
would all do it,” says Mavericks trainer Casey Smith. “Sleep does all of
those things.”
So
it was last season that Iguodala became one of several Warriors to wear
the UP by Jawbone, a wristband weighing less than an ounce and covered
in rubber that monitors sleep habits by tracking the arm’s slightest
movements. (Before the availability of such devices — and the ensuing
graphs illustrating quantity and quality of sleep — teams could only
gather data from questionnaires. “And one thing we’ve found out,” Lyles
says, “is that guys who used to say that they got nine hours of sleep
every night actually got more like five.”) Iguodala also agreed to a
no-screens-in-bed policy under Lyles and now bans his beloved TV from
his bedroom. He stores his cellphone in the bathroom overnight. He keeps
the temperature at precisely 57 degrees, to lower his body’s core
temperature. His game-day naps have been cut down to an hour. His new
in-season routine, which begins at 11:15 p.m., proceeds as follows:
stretch; do breathing exercises; read a book for 15 to 20 minutes;
lights out by midnight; repeat.
“Once
guys get a feeling for performing at a higher level,” says Jeremy
Holsopple, the Mavericks’ athletic-performance director, “it’s a big
difference from feeling like s—. Which they didn’t even think was
feeling like s—.”
Dallas
managed its own sleep program last season, inspecting rest in two-week
blocks with a motion-detecting watch called a Readiband. Five franchises
— three of them playoff teams — also convinced players to wear a
skin-adhesive, torso-mounted sensor that is colloquially known within
front offices as “the patch.” The device tracks sleep habits but also
skin temperature, body position and heart-rate variability (which is
linked to stress). As a result, the patch can discern when a player
pulls on the covers at night, when he lies down, when his pulse races
and — on account of alcohol’s observable effect on heartbeat — when he
passes out drunk.
If
it sounds like the technocratic normalizing of surveillance, it is.
“It’s part of a growing trend of employers trying to take a peek into
personal lives,” says Dr. Arthur L. Caplan, the director of New York
University’s medical ethics division and the co-director of its Sports
and Society Program. “But there are slippery-slope risks. Goals can
easily slide from improving performance to preventing you from putting
yourself at risk to making sure you don’t do anything to embarrass the
team. I’d be very, very cautious.”
Yes,
Iguodala, a star veteran with a $48 million contract, may now feel
confident experimenting with sleep under the guidance of the Warriors.
But what happens later, as the program becomes more established and a
scrub is presented with the choice to volunteer? “‘Voluntary’ is a must,
and I’m sure some teams mean it,” Caplan says. “But there’s still a
huge difference in job security between a superstar and a marginal
player. If you’re the 12th guy on an NBA bench, you probably don’t feel
quite as free to say no.”
JEREMY
HOLSOPPLE IS standing on the third floor of Chicago’s Palmer House
Hilton on a bright May afternoon. The National Basketball Strength and
Conditioning Association’s annual vendor show is in full swing, and all
around him, 39 companies flash terms like “astronaut-tested,”
“body-scanning” and “cell systems.” At one table, Alex McKechnie, the
Raptors’ assistant coach and director of sports science, grouses about
user interface with an inventor of heart monitors. At another, Bryan
Doo, the Celtics’ strength-and-conditioning coach, inquires about a
headset that interprets electrochemical brain activity. But what most
intrigues Holsopple, entering his second season in Dallas, is relatively
simple.
“Fatigue
and load are the biggest things we’re looking at right now,” he says.
“I think you can honestly say that teams lose 10 to 15 games a year
because players aren’t even remotely close to physical and mental
freshness.”
If
SportVU cameras and GPS trackers have proved anything about on-court
behavior, it is that basketball time is hardly created equal. A minute
of Thunder guard Russell Westbrook, who starts and stops like a
Lamborghini in the open floor, is nothing like a minute of center
Kendrick Perkins, a moving van who all but beeps while backing into the
paint. The true load exacted on a player’s body is a physics equation
that varies based on mass, distance, speed and acceleration. And it
applies whenever they are doing anything, anywhere; a power forward who
takes boxing lessons after work unmistakably adds to the cumulative
fatigue on his body. “Practice is only part of a 24-hour day,” says
Lyles. “Solely using that as our gauge for how much or how little we
should be doing with guys probably isn’t a very good way to do it.”
Enter
the patch, made by Proteus Digital Health. Far more than just a sleep
monitor, the patch also boasts the capacity to continuously collect
accelerometer data — and wirelessly transmit it onto a team-owned phone
or computer. Weighing 9.5 grams, the gray 4-inch oval can be stuck to
the skin and forgotten about in the process. Todd Thompson, Proteus’ VP
of corporate development, contends that without the patch’s access to
and analysis of off-court player movements, any coaching staff that
adjusts practice intensities and travel schedules does so on perilously
incomplete information.
Imagine
an NBA season as a horizontal graph of the load on a player’s body,
dotted with strategically chosen peaks (for games of the utmost
importance) and valleys (where rest is necessary to cut down the odds of
injury). Imagine the capacity to generate an all-encompassing version
of that graph, down to the hour a player tired himself out chasing his
kids in his backyard — or doing something significantly less
family-friendly. Imagine a sortable chart that lists, for each rung of
the depth chart, a color-coded number representing current overall
fatigue level. The market for that kind of risk-management solution is
self-evident.
“General
managers, owners, presidents, they’re all looking at how much money
they’re losing due to sports injuries,” says Suns trainer Aaron Nelson.
According to a recent study by Rotowire, the average NBA team
hemorrhages about $10 million in guaranteed salary from games missed due
to injury alone. This makes fatigue, which directly relates to the twin
dangers of overexertion and soft-tissue damage, a chief threat to
playoff chances and literal fortunes.
But
with a big enough cache of data? A training staff could generate
algorithmically individualized prescriptions for rest and movement. It
could act pre-emptively, based on probability on top of past results.
“The more we can objectify what guys are doing,” Lyles says, “the more
accurately we can make recommendations or change what we do.”
Change
what they do — as in benching a starter before he suffers a projected
injury. Or trading him away for that same reason. Or cutting a backup
because of a suspiciously consistent spike in fatigue level after 2 in
the morning on road trips. In which case each player should answer a
question that everyone, regardless of occupation, might soon consider
for themselves: Would you be better served, economically, by your
employer’s knowing more or less?
“They’ll
bring guys in and work them out and be able to see if they’re at a
bigger risk to hurt their knee or whatever,” says Mavericks forward
Brandan Wright.
So when it comes to contract negotiations?
“Honestly, I think it’ll hurt guys,” Wright continues. “I think that’s where it’s headed.”
THE
SPECTRUM OF NBA lifestyles is contained within one 12-foot stretch of
the Heat locker room on a March afternoon last season. On one end, Ray
Allen is explaining how he can no longer drink soda without gagging.
Seriously. The 39-year-old has gone paleo, meaning that the guard eats
mostly lean meats, fish, nuts, vegetables and fruit. All of three
lockers away stands 25-year-old journeyman Michael Beasley, whose
culinary approach involves emptying a 41-ounce bag of Tropical Skittles
into his mouth like a cement mixer filling a ditch.
Allen
eagerly embraces food as fuel for the machine. But in the tradition of
fellow pros such as Pistons forward Caron Butler — who once kept six
fridges full of Mountain Dew at home and drank a liter of it over the
course of every game — Beasley might be an equally established
basketball archetype. Which is conspicuously suboptimal.
“A
lot of guys think they can get away with it,” says Graham, the
Grizzlies’ trainer. “I’ll still get bitched at because I’m like, ‘I’m
not giving you chicken wings.'”
What
players choose to put inside their bodies has long been an agenda item
inside locker rooms. Many teams, in fact, supply meals at work. Sixers
trainer Kevin Johnson even organizes color-coded eating groups, sorted
by whose weight needs to rise (red), maintain (white) or drop (blue).
But the precision of any dietary profile is hampered without knowledge
of the way particular foods interact with particular bodies. And the
barrier to that information is the drawing of blood: a ubiquitous
practice in the English Premier League but one typically found in
American sports only as part of lab work for a regular physical.
Unless,
of course, you happen to play for a team like the Mavericks. “I think
the smartest thing we do for health from a data perspective,” says
Cuban, “is take ongoing assessments and even blood tests so we have a
baseline for each individual that we can monitor for any abnormalities.
When someone is ill, we know what their numbers should be.”
The
Mavs are adamant: They have not done — or asked their players to do —
anything illicit in the administration of these tests and the handling
of the resulting samples. Still, granting any extra permission to a vein
requires trust that an employer will analyze only what you ask them to
detect. It requires trust that possible financial incentives to run
in-season tests for a battery of performance-related substances and
conditions — anything from marijuana to hormones to herpes — will be
ignored. “I’m not saying it’s bad for a topflight athlete to be
monitored,” says Caplan, the NYU bioethicist. “But a team physician, I’m
constantly reminded, is conflicted.”
When
asked by ESPN to elaborate on blood analysis, Cuban declined further
comment. But interviews with several Dallas players indicate that the
team’s expanded testing policy is neither obvious nor rosterwide. Guard
Devin Harris recalls giving blood only in the preseason as part of the
standard team physical; perhaps by design, other plasma-related details
remain vague. “I don’t know what they do with it once they have it, but
they definitely take it,” Harris says. “And I know they talked about
taking blood throughout the season for certain stuff.”
In
the field of nutritional analysis, the payoff for a blood draw comes
when a company such as Cell Science Systems — in attendance at the
NBSCA vendor show — generates a one-page, color-coded report that
indicates whether a player has any debilitating food allergies or
sensitivities to any of 100 specific foods. A universe of dining threats
is identified. A parallel test can also be run for allergies to tattoo
ink, which one Western Conference executive says were discovered in the
case of at least one unknowingly poison-decorated player.
THERE
IS ANOTHER, decidedly less generous view of where this road goes,
however. And one day last spring, after logging 13 years in the league, a
teammate of Allen and Beasley declares that the increase in biological
testing played a role in his decision to bow out of the business
altogether. “I think all fluids will be extracted in five years,”
forward Shane Battier says, three months before officially announcing
his retirement. “I’m glad I’m done.” Battier grants that certain
archetypes — your Allens, your Iguodalas — might be perfectly willing
to revamp their private lives in the service of basketball. But, he
continues, “big data is scary because you don’t know where it’s going
and who’s seen it. I’m not saying that they’d sell research to anyone,
but I don’t trust where my blood sample will end up and what eyes will
look at it and what people outside the NBA will know about it.”
Mind
you: This is Shane Battier talking, a 36-year-old guy whose vices
lately include pizza and a carafe of Scarecrow cabernet before bed; he’s
hardly the type of libertine to employ a Whizzinator to pass a drug
test. Regardless, the very notion of evading detection may soon be
obsolete. Dr. Saxon, of USC’s Center for Body Computing, is in the
planning stages of an invention that would render the Whizzinator-esque
technologies moot. Her vision? “Minimally invasive implantables,” Saxon
says, sounding genuinely excited. “Injectable, stays in the body for a
year or two. No fuss.” She can imagine the device feeding key biometric
information to your phone. Automated directions — the equivalent of
your new car telling you to fill up the tank — would then pop up as
alerts.
“If
they ask me to put a chip in my body, I don’t know about that,” Brandan
Wright says. “I don’t want to be a complete lab rat. I already feel
like one now. I don’t want to take it to the next level.” Or, as
Mavericks center Tyson Chandler, who won a championship with Dallas in
2011, puts it, “I’m not down with the alien stuff.” Chandler, 32, might
well retire before the “alien stuff” comes to pass. But if so, he’ll
likely have to do so soon.
“We
want to be one step beyond what anyone else is doing,” says Kings owner
Vivek Ranadive, whose personal fortune was built on the comprehensive
digitization of Wall Street. “Amazingly, what banks and trading floors
were 20 years ago, sports is now. The stakes are huge, and we can act
quickly.” Just listen to his GM, who is thinking far deeper than mere
skin. “The holy grail,” D’Alessandro says, “is sequencing and
understanding the genome. And how that relates to pro athletes on an
injury basis and who’s naturally good at certain sports.” As part of his
mandate with the Kings, he’s consulted scientists about one day
building a vast predraft database of player DNA — not just for
evaluation but for gauging injury risks and prevention. “You wouldn’t
have to be identified as a person,” he says, “you could be identified as
a number. I don’t suspect this will happen in our lifetimes. But the
way things have proliferated scientifically? Maybe it will.”
History
predicts serious pushback. In 2005, Alan Milstein represented Eddy
Curry against the Bulls, whose management wanted the center to submit to
genetic screening because of an irregular heartbeat. (Curry was
eventually traded to the Knicks, bypassing the issue.) The core
objection then, as now, was that genetic markers are not actual proof of
alcoholism, or Alzheimer’s, or cancer; they just signal greater odds of
developing those conditions. In fact, as of the 2008 passing of the
Genetic Information Nondiscrimination Act, it is illegal for employers
to discriminate based on genetic information for that very reason.
Choosing to privilege reality over probability in that way, Milstein
notes, “was one of the few situations where Congress was actually
unanimous.”
In
their defense, NBA execs, team staffers and inventors do seem to
recognize these fears and offer counterarguments without being prompted.
Graham stresses that his interest as a trainer isn’t to find out how
his players entertain themselves at night, although that information may
well cross his transom — it’s to make them healthier and maximize
their careers. Holsopple, meanwhile, goes so far as to make Mavericks
players an explicit promise before sensitive monitoring takes place. “I
tell them that nobody sees the data but me and the people directly on
staff that work for me,” he says. The coaching staff, on the other hand,
“will get what they need to make decisions as coaches. But we will not
give them the things that players can be judged upon.”
Such
is the line, precarious as it is, that NBA teams are pledging to walk.
And such is the line that players, whose union will have biometrics on
its list of priorities during collective-bargaining-agreement talks in
2017, might ultimately refuse. But to hear the proponents of this
revolution tell it, they’re not so much sprinting toward Orwell as they
are grinding their way to incremental improvements. “That’s what the
reality is,” Lyles says. “We want to fine-tune things. If we do minor,
little tweaks here and there, maybe a guy doesn’t pull his hamstring.”
Or maybe, at the end of the fourth quarter, a foul defending a
game-winning shot instead becomes a block.
That
much optimization, the upside of so much technocracy, is the carrot
currently incentivizing the 30-year-old Iguodala as he staves off
departure from the game he dearly loves. In the meantime? “I just hope
we don’t become robots,” Iguodala says, “where they’re feeding us the
same thing, every day, and then it’s time to flip the switch and go to
sleep.”
That, after all, would be a different game entirely.
allow our cells to divide without dropping genes essential for life. In
this way, they are prime indicators of aging. They have been compared
to the aglets or plastic tips found at the ends of shoelaces or the wire
nuts used to protect and hold spliced electrical wires together. These
DNA sequences are responsible for what has been termed the Hayflick
Limit; the top number of divisions a human cell can have before it stops
replicating, becoming senescent or apoptotic. This process actually
protects us from unrestrained cellular division and, potentially, from
cancer.
become shorter over time with recurring replication as well as from
oxidative stress and can only be replenished via telomerase enzyme
adding back these telomeric repeats to the ends of the chromosome. Lack
of this enzyme allows inordinate telomeric shortening associated with
rapid aging and aging related health challenges. They act as a biomarker
of aging, sort of a cellular clock.
telomeres have also been linked to cardiovascular disease, some
cancers, osteoporosis, dementia, diabetes, and other chronic
degenerative diseases of aging conditions.
test is designed for anyone interested in optimal health, age
management and in knowing their telomere length as it relates to being
within or outside the normal reference range for their chronological
age.
shortened telomere length may be indicative of some chronic
degenerative medical issue occurring and possibly accelerated aging.
Telomere shortening is a dynamic process. Since telomeres respond
positively to improved dietary and lifestyle choices as well as
decreased oxidative stress knowing where their telomere sits in regards
to reference range will allow those with shorter telomeres for their age
to have the potential to change their lives, retard the hastened rate
of their telomeres shortening and potentially extend their lifespan.
Ogami, Yoshihiro Ikura, Masahiko Ohsawa, Toshihiko Matsuo, Soichiro
Kayo, Noriko Yoshimi, Eishu Hai, Nobuyuki Shirai, Shoichi Ehara, Ryushi
Komatsu, Takahiko,Naruko and Makiko Ueda