All eyeMDs agree that Non-Preserved or Preservative Free is the best as long term preservatives seem to damage delicate ocular cells. Dry eye and allergy go hand in hand with each making the other worse often. Itching is a key component of allergy or Demodex mites on the eyelashes. Some drops in both Category A & B may be needed for any symptom of dryness, itching, tearing (often reflex tearing to dryness), redness, foreign body sensation, blurry vision (that comes & goes), swelling, eye pain, orbital pain, eyelid twitching, eye-straining.
A. Category A. Drops for DRY EYES:
1st Generation Artificial Tears: not recommended
1.Collyrium: “eye wash.” The notoriously famous cobalt blue glass bottle, equipped with an 2. Saline-based, isotonic or hypotonic tears with preservatives, notably benzalkonium chloride.
– short retention time
-transient relief
-requires high frequency of instillations
-allergy to preservative common
2nd Generation Artificial Tears: Natural Polymers (Methylcellulose Derivatives) and Synthetic Polymers (e.g., polyethylene glycol, polyvinyl alcohol, povidone, carbopol, polyguar and HP guar)
-higher viscosity
– better retention time than preceding components, and are still included in products like Systane (Alcon) and Refresh Optive (Allergan). The drawback to some of these gel-forming drops is that the improvement in symptoms was at times accompanied by a transient visual blurring. These products also introduced the concept of gentler preservatives or even preservative-free tears, giving patients with sensitivities or allergies additional options.
3nd Generation Artificial Tears: Hyaluronic acid tears
–Hyaluronic acid is a naturally occurring polysaccharide in the human body.
-found in connective tissue, vitreous, and aqueous humor: coats the corneal endothelium.
-Increased viscoelasticity of the polysaccharide leads to increased tear stability, reduction of tear removal, protective effects on the corneal epithelium and consequently, a reduction in many dry-eye symptoms.11-13
–Cross-linked HA applied t.i.d. significantly improved ocular surface health compared to a standard HA-containing tear in dogs with a clinical diagnosis of dry eye.14
–0.3% sodium hyaluronate had a significantly longer retention time than other lubricants, including carboxymethylcellulose and hydroxypropyl methylcellulose.15
-Examples:
1. Blink Tears (Abbott Medical Optics) The Still, the viscoelasticity of HA-based products varies significantly, depending on molecular weight and HA concentration. Covalently crosslinking HA generates a more viscoelastic material in comparison to original HA-based tear supplements that have a low concentration of high-molecular-weight HA. One study found that the
4nd Generation Artificial Tears: Lipid Emulsions/Omega 3
-lipid oil-in-water nano-emulsions have a long residence time on the tear film, reduce the tear evaporation rate and have a positive effect on the lipid layer.16,17
-Nano-emulsions also improve ocular bioavailability of lipophilic or poorly water-soluble drugs.18
-These tears need “surface active agents,” or surfactants to stabilize them, which commonly create a negatively charged preparation.
-Examples:
1. Soothe XP (Bausch + Lomb)
2. Systane Balance (Alcon)
3. Retaine (Ocusoft) is a unique preservative-free artificial tear option containing a proprietary cationic oil-in-water nano-emulsion with novel bio-adhesive properties. It’s thought that electrostatic interactions between the positively charged oil nano-droplets and the negatively charged ocular surface epithelium increase the residence time on the ocular surface, thereby enhancing the protection and restoration of a healthy tear film and corneal epithelium.17,18
4. REFRESH OPTIVE MEGA-3®.
- Preservative-free, low blur formula fortifies and restores the lipid layer. Its unique blend of natural oils helps prevent tear evaporation.
- Treats Dry Eye signs and symptoms associated with Meibomian Gland Dysfunction (MGD).
- Nourishes all three layers of the tear film damaged by Dry Eye for immediate, long-lasting relief.
a. pheniramine,
b. antazoline,
c. chlorpheniramine
d. cyclizine.
2. Mast Cell Stabilizers
I hope this helps.
Sandy Cremers, MD, FACS
References:
1. https://www.aaaai.org/conditions-and-treatments/drug-guide/eye-medications
|
Eye Drops
|
||||
|
Generic Name
|
Brand Name
|
Class
|
Dosage
|
Tips and Product Links (if available)
|
|
Alcaftadine 0.25%
|
Lastacaft
|
Allergic Conjunctivitis
|
3 y/o and above 1 drop each eye once a day
|
|
|
Azelastine
|
Optivar
|
Azelastine is classified pharmacologically as a second-generation antihistamine, ie, it is a relatively selective, nonsedating, competitive antagonist at H1 receptors. Its relative lack of central nervous system activity distinguishes it from first-generation antihistamines. Inhibition of inflammatory mediators, in addition to antihistaminic and mast cell stabilizing effects, place it among the new generation of dual-acting anti-inflammatory drugs. In addition to azelastine’s high affinity for H1 receptors, its ability to modify several other mediators of inflammation and allergy contributes to its mechanism of action.8 In vitro and in vivo studies, as well as the clinical trials discussed here, support the dual effects of direct inhibition and stabilization of inflammatory cells: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2938280/
|
1 drop each affected eye twice a day.
|
Same medication that is in Astelin Nasal Spray.
|
|
Bepotastine 1.5%
|
Bepreve
|
Allergic Conjunctivitis
|
3 y/o and above 1 drop each eye twice daily
|
|
|
Cromolyn
|
Crolom and
Generic/OTC Cromolyn |
Mast Cell Stabilizers
|
1 drop each affected eye 4 to 6 times a day.
|
|
|
Emadastine
|
Emadine
|
Antihistamines: Emedastine (trade name Emadine) is a second generation[citation needed] antihistamine used in eye drops to alleviate the symptoms of allergic conjunctivitis. It acts as a H1 receptor antagonist. It works by blocking the action of histamine that causes allergic symptoms. It is used in form of the difumarate.[1] The emedastine difumarate is a white, crystalline, water-soluble fine powder. Emedastine eye drops is usually applied twice a day to the affected eye. When the patients with allergic conjunctivitis were treated with 0.05% emedastine difumarate ophthalmic solution for six weeks, the signs and symptoms such as redness, itching and swelling of the eyes were relieved: Wilkipedia
|
1 drop each affected eye up to 4 times a day.
|
|
|
Epinastine
|
Elestat
|
Antihistamine/
Mast Cell Stabilizers |
1 drop each eye twice a day.
|
|
|
Ketorolac
|
Acular
|
Non-steroidal Anti-inflammatory Drug
|
1 drop in each affected eye 4 times a day.
|
|
|
Ketotifen
|
Zaditor
Alaway OTC Zyrtec |
Antihistamine/
Mast Cell Stabilizers |
1 drop every 8 to 12 hours.
|
|
|
Lodoxamine
|
Alomide
|
Mast Cell Stabilizers
|
1 or 2 drops into each affected eye 4 times daily for up to 3 months.
|
|
|
Loteprednol 0.2%
|
Alrex
|
Corticosteroids
|
1 drop into the affected eye up to 4 times a day.
|
|
|
Loteprednol 0.5%
|
Lotemax
|
Corticosteroids
|
1 to 2 drops 4 times a day.
|
|
|
Naphazoline
|
AK-Con
Vasocon Albalon and many generic versions. OTC |
Decongestants
|
1 drop into affected eye every 4 hours up to 72 hours of use.
|
|
|
Naphazoline/
Pheniramine |
Naphcon A
Opcon-A Visine-A OTC Store brands |
Antihistamine/
Decongestants |
1 to 2 drops each affected eye up to 4 times a day.
|
|
|
Nedocromil
|
Alocril
|
Mast Cell Stabilizers
|
1 or 2 drops in each affected eye twice a day.
|
|
|
Olopatadine
|
Patanol 0.1%
|
Antihistamine/
Mast Cell Stabilizers |
1 drop in each eye twice a day at an interval of 6 to 8 hours.
|
|
|
Pataday 0.2%
|
Antihistamine/
Mast Cell Stabilizers |
1 drop each eye once a day.
|
||
|
Olopatadine HCL 0.7%
|
Pazeo
|
Allergic conjunctivitis 2 years and older
|
1 drop each eye once a day
|
|
|
Pemirolast
|
Alamast
|
Mast Cell Stabilizers
|
1 or 2 drops in each affected eye 4 times a day.
|
|
2. https://www.sciencedirect.com/topics/medicine-and-dentistry/alcaftadine
2. Journal of Ocular Pharmacology and Therapeutics
3.
PUBLISHED 8 DECEMBER 2014
3,500 Years of Artificial Tears
After three millennia of battling the discomfort and irritation of dry eye, is ophthalmology any closer to a solution?
— Prescription from Assyro-Babylonian ophthalmology1
Based on the quote above, it seems we’ve been trying to find relief from dry eye for quite a long time. In 1872, Georg Ebers, a German Egyptologist, discovered a collection of Egyptian medicinal recipes later called the Ebers Papyrus, written sometime between 1553 and 1550 B.C.2 Eye pastes with exotic elemental ingredients such as antimony, copper or manganese were referenced throughout the document as anti-infectives, sunscreens or cosmetics.3 We’ve come a long way since then, but dry eye still remains one of the more challenging diseases to treat. With only one drug (Restasis, Allergan) earning Food and Drug Administration approval to date, we are left with a potpourri of artificial tears to address this unmet need. A visit to any local pharmacy will find shelves of drops, lubricants and gels all offering symptomatic relief for dry-eye sufferers. Although these are not the cures we might hope for, the artificial tears of today are a long way from both the yellow frog gal of ancient Egypt and the saline drops that were the first modern tear replacements. Many artificial tears available today reliably mimic real human tears, and several may actually outperform their natural counterparts. In this month’s column, we’ll provide an assessment of the current artificial tear landscape, and take a look at how formulations have evolved to optimize hydration and lubrication.
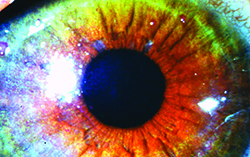
The Tear Film and Blink
A healthy, stable tear film provides a smooth protective layer over the corneal surface that’s essential for good vision and ocular comfort.4 Conventionally, the tear film is thought to be composed of three layers: an outer lipid layer (~ 0.1 µm thick) produced by the meibomian glands in the tarsal plate; a central aqueous layer (~ 7 to 10 µm thick) produced by both the main and accessory lacrimal glands; and an inner mucin layer (~ 0.2 to 1.0 µm thick) produced by goblet cells in the conjunctiva.4-7
|
Recent work has amended this three-layer architecture with the concept of an integrated aqueous and mucin layer. While mucins concentrate close to the ocular surface, a significant amount of mucin, particularly mucin 5A, is distributed throughout the aqueous tear film.5-7 Still, this triple-layer structure remains useful in understanding the multitasking of the tear film and the pathophysiology of dry eye. At the molecular level, the list of components could fill volumes, and includes water, electrolytes, antimicrobial molecules and several peptide growth factors.7 This is just a small sample of a tear component list that includes many more constituents found in vanishingly small amounts, each playing some role in maintaining a healthy ocular surface. Among these roles are constant hydration of the cornea and conjunctiva; protection of the ocular surface from dust, dirt particles or foreign bodies; and maintenance of corneal transparency for clear vision. Tears also provide a source of nutrients for the avascular cornea. When the quality or quantity of tears is compromised by an imbalance or breakdown in any of these components, it can severely impact the eye and cause or exacerbate dry-eye symptoms.5,6
The tear film is not a static entity, but rather is in a state of constant flux, with each blink forcing a fraction of the total volume out through sinus canalicular drainage to be replaced by lacrimal, meibomian and goblet cell secretions. The tear film’s life cycle spans the time between two blinks, and its deterioration and eventual breakup initiate the next blink. Measuring tear-film breakup time, visualized with fluorescein, is a standard assessment of tear-film health. A more integrative assessment of the tear film used in clinical research, called the ocular protection index, is a ratio of blink rate over breakup time.8 Ideally, blinks replenish a healthy tear film prior to significant breakup, and an unstable tear film can prompt blinking at a faster rate, one of the known consequences of dry eye. The OPI score reflects this anomaly: in a subject with an OPI < 1, breakup time is shorter than blink rate, leading to an exposed, compromised ocular surface. Conversely, a subject with an OPI score > 1 reflects a healthy tear dynamic where blinks precede the breakup of the aging tear film.
Dysfunction of any component of tears can lead to tear film instability, ocular surface exposure and dry eye. Inadequate lubrication results in ocular surface damage, discomfort and compromised visual function, all of which can negatively affect the patient to varying degrees, often drastically reducing quality of life. Many external and internal factors play a role in the development or exacerbation of dry eye. Visually intensive situations like working on a computer, reading or driving at night can contribute to a hyper-stressed tear film as the blink rate is reduced by concentration. Certain medications, systemic diseases, contact lens use, ocular allergy, refractive surgery, age and gender are also risk factors for the disease. In order to supplement a deficient tear film, tear substitutes are commonly used as a first line of defense.
The Challenge
Current prevalence of dry eye in the United States has been conservatively estimated at somewhere between 6 and 10 million people;9 other projections suggest as many as 11 percent of adult men and 17 percent of adult women are affected.6 These rates will undoubtedly grow in the next 10 to 20 years as the population ages. As the mainstay of therapy for dry eye, the artificial tear market is projected to reach $2 billion globally by 2018. This is not the result of a blockbuster success story, rather it’s a reflection of the failure of any single product to provide relief for more than a fraction of dry-eye sufferers.7
One of the most significant challenges for all topical products is that they are rapidly eliminated from the ocular surface by a variety of barrier functions. Even when tear function is compromised, newly secreted tears are still acting to dilute and wash away active agents from added drops, while blinking exchanges the existing tear film and removes instilled tear substitutes by continuously pushing the tears into marginal menisci and punctal openings. Finally, the sensitivity of the cornea to minute changes in pH and osmolarity resulting from eye-drop instillation induce reflex blinking and tearing, further preventing a therapeutic benefit from artificial tears. We see that any artificial tear fights an uphill battle with regard to residence time. The key challenge is to develop a formulation that would remain longer on the ocular surface and thus provide a more sustained therapeutic effect.
When posing the question of what makes a good drop, the symptomology of dry eye provides a checklist of therapeutic targets. Drops should reduce burning, improve reading speed and comprehension and normalize blink pattern and frequency. These are all factors that our patients will perceive, and even if they can’t identify the specific effects of the drops, we can quantify the changes in the clinic and use them as a guide in eye-drop development. An example of this is the inter-blink interval visual acuity decay test. The decline in acuity measured with IVAD is greater in those with dry eye than normal controls, but it can be normalized with artificial tears.10
Generations of Artificial Tears
Over the years, we’ve seen many artificial tears come and go on the market, often calling themselves a “next-generation” product. The modern history of artificial tears can be traced back to the days of the traveling medicine show with a product Collyrium, a word that literally translates from Latin as “eye wash.” The notoriously famous cobalt blue glass bottle, equipped with an eye-cup top, was designed to make users’ “eyes right” by relief from strain or irritation by dust or wind. The eye-cup bath was a popular delivery system for instilling liquid medications onto the eye until the more traditional screw-capped tops emerged. These early attempts at dry-eye relief were followed by a generation of tear substitutes that were saline-based, isotonic or hypotonic solutions with preservatives, notably benzalkonium chloride. Generally speaking, these artificial tears spread poorly across the ocular surface and their short retention time led to transient relief and very high frequency of instillations.
Jump ahead to the 1980s, and there came a boom in the advancement of artificial tears. This next generation integrated natural polymers (e.g., methylcellulose derivatives) and synthetic polymers (e.g., polyethylene glycol, polyvinyl alcohol, povidone, carbopol, polyguar and HP guar) into artificial tear formulations. All these polymers added a higher viscosity, offering a better retention time than preceding components, and are still included in products like Systane (Alcon) and Refresh Optive (Allergan). The drawback to some of these gel-forming drops is that the improvement in symptoms was at times accompanied by a transient visual blurring. These products also introduced the concept of gentler preservatives or even preservative-free tears, giving patients with sensitivities or allergies additional options.
Hyaluronic acid tears are considered to be the third generation of dry eye artificial tear therapy. HA is a naturally occurring polysaccharide in the human body. While it is found mainly in connective tissue, it is also highly concentrated in the vitreous, and in the aqueous humor where it coats the corneal endothelium. Products such as Blink Tears (Abbott Medical Optics) are set apart by their hyaluronic acid content. The viscoelasticity of the polysaccharide leads to increased tear stability, reduction of tear removal, protective effects on the corneal epithelium and consequently, a reduction in many dry-eye symptoms.11-13 Still, the viscoelasticity of HA-based products varies significantly, depending on molecular weight and HA concentration. Covalently crosslinking HA generates a more viscoelastic material in comparison to original HA-based tear supplements that have a low concentration of high-molecular-weight HA. One study found that the cross-linked HA applied t.i.d. significantly improved ocular surface health compared to a standard HA-containing tear in dogs with a clinical diagnosis of dry eye.14 A second study comparing the in vivo efficacy of several ocular lubricants in rat and rabbit animal models of dry eye found that 0.3% sodium hyaluronate had a significantly longer retention time than other lubricants, including carboxymethylcellulose and hydroxypropyl methylcellulose.15
It’s not surprising in light of this discussion that one of the top complaints of patients is that artificial tears don’t last long enough. The main benefit of the latest generation of tears addresses this very issue. Most recently, we’ve seen the introduction of lipid emulsions into the artificial tear arena. Considered the fourth and most advanced generation of artificial tears, lipid oil-in-water nano-emulsions have been shown to have a long residence time on the tear film, reduce the tear evaporation rate and have a positive effect on the lipid layer.16,17 Nano-emulsions also improve ocular bioavailability of lipophilic or poorly water-soluble drugs.18 Generally emulsions need “surface active agents,” or surfactants to stabilize them, which commonly create a negatively charged preparation. Several emulsion-based products exist on the market to-date, including Soothe XP (Bausch + Lomb) and Systane Balance (Alcon). Retaine (Ocusoft) is a unique preservative-free artificial tear option containing a proprietary cationic oil-in-water nano-emulsion with novel bio-adhesive properties. It’s thought that electrostatic interactions between the positively charged oil nano-droplets and the negatively charged ocular surface epithelium increase the residence time on the ocular surface, thereby enhancing the protection and restoration of a healthy tear film and corneal epithelium.17,18
Beyond Eye Drops
While it seems that artificial tears will always be a feasible first line of defense for dry-eye sufferers, there continues to be a push for alternative options. Several recent studies focus specifically on one aspect of dry-eye disease: lacrimal gland dysfunction. One of these involves restoration of lacrimal function by transplanting (or, in the case of the parotid gland, rerouting) minor salivary glands, but these procedures yielded a hypo-osmotic tear composition and subsequent epithelial edema.19 More recent studies have examined development of bioengineered tear-forming glands. In a mouse model that mimics the ocular surface damage of dry eye, duct integration of an orthotopic engraftment of a bioengineered lacrimal gland germ into an adult extraorbital gland-defect model mouse indicated that the bioengineered lacrimal gland replacement can restore the physiological functions of the lacrimal gland, including the production of sufficient volume of an appropriate tear and protection of the ocular surface.20
A second strategy aimed at enhancing lacrimal gland function employs autologous platelet-rich plasma. While serum has been used to supplement topical treatments in the past, this new strategy employs PRP in situ, liberating a host of biologically active proteins, promoting cell recruitment, growth and differentiation. The technique has been used successfully for treatments including wound closure, corneal ulcers, chemical burns and skin rejuvenation. Beneficial effects have been observed for epithelial recovery in post-LASIK corneas and in severe dry eye.21,22 A recently published pilot study in patients with severe lacrimal dysfunction and dry eye showed that lacrimal injections of PRP were found to be safe and effective in increasing lacrimal production and in reducing ocular staining.23
These experimental strategies are likely to be used only in the most severe cases of dry eye. For the majority of dry-eye sufferers, topicals such as artificial tears will continue to be the treatments of choice in a cost-benefit based therapeutic landscape. Still, with the improvements in today’s artificial tears, there’s no doubt that dry-eye patients are seeing greater choices and more effective products than those of generations past. We’ve seen that we can do better than yellow frog gal but we also know that there’s plenty of room for more progress, particularly in the area of agents that provide greater relief for moderate to severe dry eye, as well as those that provide a greater duration of relief. After 3,500 years of being in the works, the thought of long-term relief for dry eye seems like a therapy whose time is long overdue. REVIEW
Dr. Abelson is a clinical professor of ophthalmology at Harvard Medical School. Ms. Lafond is a medical writer at Ora Inc.