Microinvasive glaucoma surgeries (MIGS) are surgeries that try to safely facilitate the removal of the eye’s liquid, called the aqueous, to the outside of the eye in efforts to lower the eye’s pressure or Intraocular pressure (IOP).
MIGS is much safer and has less risks than standard bleb-based surgical procedures for glaucoma: these have a much longer recovery and a much higher risk of infection, endophthalmitis, and loss of the eye.
There are 3 key MIGS procedures used by the majority of US surgeons:
1. Goniotomy performed using the Kahook Dual Blade (KDB) (New World Medical, Rancho Cucamonga, CA, USA) and
2. iStent trabecular bypass device (Glaukos, San Clemente, CA, USA).
3. Cypass: which was taken off the market 8/29/2018 due to concern about long term effects on endothelial cell counts which keep the cornea clear long term.
The only published paper having a head to head comparison between Goniotomy and iStent was sponsored by the Goniotomy company started by Dr. Kahook: obviously they say they are better.
It will take larger randomized trials without corporate funds to see which is really the best for most patients. For now, it is likely they are similar in long term outcomes with Goniotomy having the longer track record in general.
At the end of this post is my Tiered Approach for how best to treat glaucoma. This is still true but would add Cypass if it is put back on market.
SLC
Clin Ophthalmol. 2018; 12: 791–797.
Published online 2018 Apr 30. doi: 10.2147/OPTH.S158403
PMCID: PMC5933398
PMID: 29750011
A multicenter retrospective comparison of goniotomy versus trabecular bypass device implantation in glaucoma patients undergoing cataract extraction
Abstract
Purpose
The aim of this study was to compare intraocular pressure (IOP) outcomes in eyes with cataract and glaucoma undergoing phacoemulsification (phaco) in combination with goniotomy using the Kahook Dual Blade (KDB) or implantation of a single iStent trabecular bypass device.
Methods
Retrospective analysis of IOP and IOP-lowering medication reduction in eyes undergoing phaco-goniotomy with KDB (n=237) or phaco-iStent (n=198). Preoperative, intraoperative, and postoperative data were collected through 6 months of follow-up. Outcome measures included mean IOP reduction, mean reduction in IOP-lowering medications, and the proportion of eyes achieving ≥20% IOP reduction or ≥1 medication reduction from baseline.
Results
Mean IOP in the phaco-goniotomy with KDB group decreased from 17.9±4.4 mmHg at baseline to 13.6±2.7 mmHg at Month 6 (P<0.001), with mean medication use decreasing from 1.7±0.9 to 0.6±1.0 (P<0.001). In the phaco-iStent group, mean IOP decreased from 16.7±4.4 mmHg to 13.9±2.7 mmHg (P<0.001), with mean IOP-lowering medication use decreasing from 1.9±0.9 to 1.0±1.0 (P<0.001). Mean IOP reduction from baseline was significantly greater in the phaco-goniotomy with KDB group at Month 6 (phaco-goniotomy with KDB −4.2 mmHg [23.7%] vs phaco-iStent −2.7 mmHg [16.4%]; P<0.001). IOP-lowering medication reduction was greater in the phaco-goniotomy with KDB group compared to the phaco-iStent group (1.1 vs 0.9 medications, respectively; P=0.001). The most common adverse event was IOP spikes occurring in 12.6% of phaco-iStent eyes and 6.3% of phaco-goniotomy with KDB eyes (P=0.024).
Conclusion
Goniotomy with the KDB combined with cataract surgery significantly lowers both IOP and the need for IOP-lowering medications compared to cataract extraction with iStent implantation in glaucomatous eyes through 6 months of postoperative follow-up.
Keywords: glaucoma, goniotomy, intraocular pressure
Footnotes
Disclosure
All authors have received research support from New World Medical in the past. No financial support was received for the work involved in this article. Drs Dorairaj, Kahook, Williamson, Seibold, and Singh are consultants for New World Medical. Dr Kahook receives royalties from licensed patents pertaining to the KDB. Dr ElMallah has no relevant financial disclosures. The authors report no other conflicts of interest in this work.
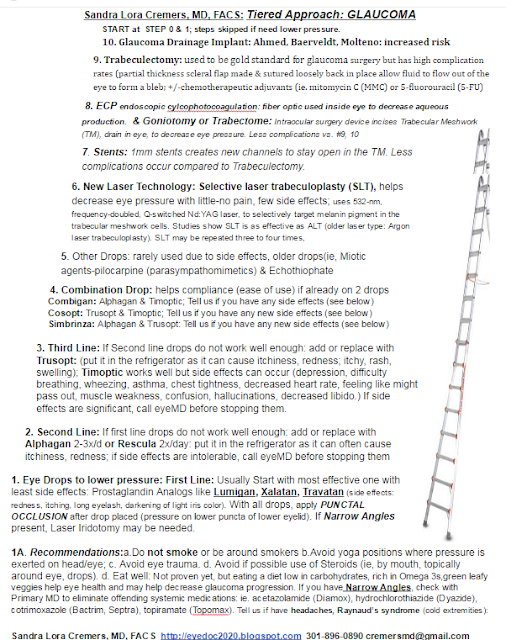
Dr. Cremers’ Tiered Approach to Glaucoma:
iSTENT:
POSTOPERATIVE CARE.
This varies by surgeon but I usually follow the below protocol:
1. Shield applied to the operative eye.
2. Post op Day 1 visit:
3. Post op Instructions:
It takes at least six weeks to reach a new steady-state baseline pressure.
We watch for a steroid response which is related to genetic risk factors.
I taper the steroids quickly if possible: four times daily for the first week; twice daily for the second week; then stop.
The average iStent patient is on 2.3 medications before surgery. For patients on two or more medications, I may continue 1 med until I am sure the eye pressure is at the patient’s “Tgoal” (ie, the Tgoal is 30% off the Tmax (maximum intraocular pressure) we calculated to see what IOP number should prevent further nerve damage).
In lower risk patients with non-advanced glaucomatous optic nervers: I may stopped all meds. If the patient is on just one medication, I usually will stop drops after a MIGS procedure but if patient is on 3 or more, I usually will keep one drop on or follow more closely to be sure IOP does not spike.
GONIOTOMY:
POSTOPERATIVE CARE. This varies by surgeon. In general, I discharge my patients with the following instruction:
1. Shield applied to the operative eye.
2. Post op Day 1 visit:
3. Post op Instructions:
- Topical antibiotic drops are given four times daily for seven days.
- Steroid drops, four times daily, are tapered over eight weeks.
- Pilocarpine (1 or 2 percent) is used in the operative eye two to four times daily, tapered over two to eight weeks. Pilocarpine is intended to minimize formation of peripheral anterior synechiae and to help with short-term IOP reduction.
- All preoperative glaucoma medications may be restarted immediately and tapered the first postoperative day, depending on IOP.