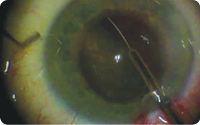
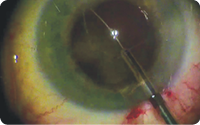
Figure. The miLoop device.

Tremendous changes in cataract surgery have occurred over the years, from the initial days of large-incision intracapsular cataract extraction to the most recent advances in small-incision laser cataract surgery. Much of the progress we have witnessed has focused on safely removing the cataractous lens through increasingly smaller incisions. Despite the many advantages of advanced cataract surgery techniques, including phacoemulsification and laser cataract surgery, surgical pitfalls still exist. It is for this reason that I recently became interested in the miLoop (IanTech; Figure), a new device designed to transect the cataractous lens with minimal energy and maximal safety. The miLoop has received FDA regulatory learance, with anticipated availability in the United States this summer.
PITFALLS IN CURRENT TECHNIQUES
Phacoemulsification with ultrasound, one of the most significant revolutions in cataract surgery to date, has allowed relatively safe lens removal through an incision even smaller than 2 mm. One disadvantage of using ultrasound, however, is that the collateral energy transferred to ocular structures can result in swelling and inflammation. Furthermore, phaco ultrasound requires technical expertise to perform, potentially requiring years of learning to master. It also entails a fixed capital expense for the machine and additional disposable costs incurred on a per-use basis, possibly limiting availability of the technology in the developing world.
Femtosecond lasers were recently developed to help increase the precision and accuracy of cataract surgery, making the procedure easier among broader skill sets. The use of a laser for key steps of surgery has helped to reduce the ultrasound energy required to remove the lens and has resulted in quicker healing. Unfortunately, the technology also drastically increases the cost of the procedure, potentially decreases the efficiency of surgery, and comes with a learning curve that requires time and experience to achieve results that are equal or superior to those achieved with standard cataract surgery. Laser cataract surgery has also made some of the surgical steps more challenging such as cortical cleanup with irrigation and aspiration (I/A).
ENTER THE MILOOP
The miLoop sidesteps some of the pitfalls associated with various cataract surgery techniques. After using the device in 40 cases, I believe in its potential to make cataract surgery safer and more efficient by drastically reducing or potentially eliminating the need for ultrasound energy.
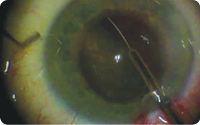
This single-use disposable instrument features a flexible, retractable, nitinol loop that is designed to be deployed within the capsular bag to encircle the cataractous lens. Once that step is complete, the loop is retracted, and the lens is effectively bisected. The loop can be redeployed multiple times at the beginning of the case to break the cataract into smaller, more manageable pieces.
The shape of the loop mirrors the natural anatomy of the capsular bag to prevent capsular damage. Furthermore, the gauge of the nitinol is stiff enough to allow manipulations within the bag to ensnare the cataract, but it is flexible enough to avoid damaging the bag and zonular structures.
The step-by-step technique that I have been using with the miLoop may be viewed on Eyetube.net (see video below) and is outlined on the following page.
William F. Wiley, MD, uses the miLoop device to transect a cataract.
ADVANTAGES
I have noticed several unique advantages to the miLoop compared with other techniques for softening and dividing the lens.
No. 1. The miLoop transects the cataract completely, without leaving an untreated area. For safety reasons and owing to technical limitations, the femtosecond laser cannot soften the lens fully to the lens equator, and a buffer zone of at least 500 µm is required between the treated area and the capsular bag.
No. 2. The miLoop can even be deployed through a relatively small pupil, ensuring the device’s potential use on nearly every cataract. On the other hand, the treatment area with femtosecond lasers is limited by the size of the pupil, because treatment cannot extend beyond the pupillary margin.
No. 3. Constriction of the miLoop slightly lifts and loosens nuclear material, allowing safe and easy removal of nuclear segments. While deployed and rotated, the device loosens the cortical material, making the I/A step of cortical removal easier. Conversely, I/A can be more challenging in a laser-treated eye, because the cortex is often closely adherent to the capsular edge.
No. 4. The miLoop works independently of the nuclear density. Because the device can cut through both soft and dense nuclei, the effect of apparent variability and the need for technique adjustments with different cataract grades are reduced. Furthermore, compared with traditional lens-dissection techniques, the miLoop appears to be gentler on the ocular structures and to require less of the manipulation and stretching of the capsular bag that are often needed with manual chopping techniques.
1
Beginning just like standard cataract surgery, a 1-mm paracentesis is created, and a dispersive ophthalmic viscosurgical device is injected. Then, a 2.5-mm clear corneal incision is created.
2
Next, the surgeon performs a centered 5.5-mm capsulorhexis, followed by routine hydrodissection.
3
The anterior chamber is then extended with additional dispersive viscoelastic, allowing proper insertion of the miLoop device (IanTech).
4
The ophthalmologist tests the miLoop instrument outside the eye to ensure proper function by deploying and then retracting the snare loop.

5
After confirming that the loop is fully retracted, the surgeon deploys the loop parallel to the iris and directs it underneath the anterior capsule. During deployment, the loop migrates between the anterior capsule and the nuclear cortex.
6
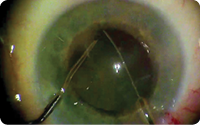
Once fully deployed, the device is rotated 90º so that the loop slides around the lens, effectively ensnaring the lens within the nitinol loop.
7
Once the cataract is completely ensnared, the loop is retracted. This bisects the lens into two equal pieces. If further dismantling is desired, the bisection process may be repeated multiple times by removing the miLoop device from the eye, rotating the lens within the capsular bag, and then reinserting the miLoop and repeating the bisection described above. Alternatively, an advanced approach to removing the loop from the eye prior to each bisection can be used. After the first bisection is created, the loop can be redeployed in the original bisection groove. Once the device is redeployed fully, the surgeon can rotate the cataract with a carousel technique within the loop to expose a new portion of the lens for dissection.
8
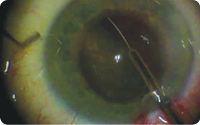
Typically, the lens is rotated 30º to 60º from the original groove, and then the loop is again retracted. This step is repeated once more by expanding the loop within the second groove, rotating the lens another 60º, and then constricting the loop.
9
At this point, the constricted loop may be carefully removed from the eye. By deploying the miLoop three times, each 60º apart, the surgeon effectively divides the cataract into six relatively equal pie-shaped pieces.
10
Once the lens has been effectively transected multiple times, the nuclear material can be removed with either a modified I/A tip or a traditional ultrasound probe. The amount of phaco energy required (if any) will depend on the density of the cataract and the amount of lens dissection performed with the miLoop.
RESULTS
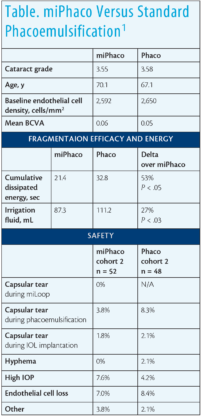
Earlier in 2017, a randomized controlled study was conducted with miLoop and phacoemulsification (miPhaco) versus standard phacoemulsification (standard phaco) in moderate to advanced cataracts. In all cases, the Centurion Vision System (Alcon) with torsional ultrasound was used for phacoemulsification. Baseline demographic data, visual outcomes, and safety were similar in the miPhaco group (n = 100) and standard phaco group (n = 100), and the average cataract grade was 3.55 and 3.58, respectively. In the cases in which the miLoop was used to fragment the lens, it was done prior to phacoemulsification.
Results are shown in the Table. In the standard phaco group, mean cumulative dissipated energy and fluidics values were 53% and 27% higher than in the miPhaco group. Further, endothelial cell loss was 20% higher in the standard phaco group (8.4% vs 7%). The researchers also found that the miLoop greatly improved peripheral cortical removal.
SYNERGIES AND OPPORTUNITIES
Although the miLoop may have the ability to displace some current technologies, there is also an opportunity for the device to work synergistically with available therapeutic options. For instance, it can be used after laser cataract surgery to assist with nuclear dissection and to help release adherent cortex during I/A. The miLoop can also work well with current phaco ultrasound, allowing more efficient and lower energy usage.
With that said, I expect the miLoop to open the door to a whole new set of technologies and approaches to cataract removal. By effectively dissecting the nucleus into small, manageable pieces, there is the potential for a tool other than traditional phacoemulsification and I/A to remove the cataract fragments. This may spur the development of even safer and more effective approaches to cataract extraction.
I can also foresee the use of the miLoop in premium cataract surgery, a procedure that promises to deliver the best outcomes and the quickest healing times. By reducing or eliminating phaco energy during the procedure, the device may allow premium patients to achieve their visual potential quicker with lower complication rates. Beyond premium cases, surgeons may prefer to use the technique in all cases if it provides a better experience for both themselves and their patients.
As a cost-effective and obtainable technology, the miLoop may provide first-world outcomes in third-world settings. Its disposable and portable nature recommends the device’s use where ophthalmologists may not have access to expensive phaco machines.
WHADDAYA THINK OF THAT?
Three surgeons respond to three questions.
QUESTIONS
1. WHAT IS YOUR IMMEDIATE REACTION TO THE MILOOP (IANTECH)?
2. IN YOUR OPINION, WHAT IS THE POTENTIAL OF THE PRODUCT?
3. WOULD YOU CONSIDER USING THE MILOOP WHEN IT BECOMES AVAILABLE? IF YOU ARE SKEPTICAL, WHY WOULDN’T YOU?

T. HUNTER NEWSOM, MD
• Newsom Eye, Tampa and Seabring, Florida
• hunter@newsomeye.net
• financial interest: none acknowledged
1. My immediate reaction was, “Why didn’t I think of this?” The miLoop is a simple device that can reduce the energy required to remove a cataract, and it can be done with a short learning curve.
2. I believe the miLoop could eliminate the need for phacoemulsification during cataract surgery. The removal of a cataract requires a certain amount of energy, and the bulk of that energy can be delivered with a femtosecond laser followed by minimal phacoemulsification or entirely with phacoemulsification. Both techniques always put energy into the eye, which requires recovery. With the miLoop, the cataract, no matter how hard, can be fragmented into smaller pieces without any energy. The miLoop also does not increase surgical time and could potentially even reduce surgical time.
3. I will definitely use the miLoop when it becomes commercially available. I have never thought of the phaco portion of cataract surgery as being a burdonsome step. However, when I used the miLoop in every other case on a 40-case day, I quickly wanted to use one every time, because phacoemulsification seemed to be more of a burden. In short, I look forward to eliminating my phaco machine from the cataract surgery procedure. Also, outside the United States where modern phaco technology is not available, the miLoop will allow removal of the densest cataracts with little effort.

1. I was aware of the technology and had previously seen videos of the miLoop being used in cataract surgery. The device is essentially a modification of the lens snare, which has been used for many years in conjunction with small-incision sutureless extracapsular cataract extraction. The difference between the devices is that the loop of the miLoop is made of nitinol, which is an alloy that has memory—in this case, the shape of the lens nucleus. The loop is slipped around the nucleus in the bag to transect it.
2. I think that there may be some use for the miLoop in very dense cataracts that are difficult to chop. The Akahoshi prechop technique and standard chopping both work well with medium nuclei. I suppose that very soft nuclei could be divided with the miLoop to facilitate removal; however, I would be concerned about damaging the edge of the capsulotomy if the opening were too small.
3. It would certainly be worth a try to see how easy the miLoop is to use in real life.

ROBERT J. WEINSTOCK, MD
• private practice, The Eye Institute of West Florida, Largo, Florida
• rjweinstock@yahoo.com
• financial interest: none acknowledged
1. I have done about 30 cases with the miLoop in all types of cataracts, from very soft to very dense. My first impression was that it was much easier to do than I expected. I was easily able to get the injector through a sub-2-mm wound, and after a few cases, I was able to perform nuclear cleaving in under 1 minute. However, it does take some skill, concentration, and a steady hand to deliver the device under the capsular edge and open it with the trigger to extend the device around the nucleus. This must be achieved while maintaining the tip of the injector in the anterior capsular plane as you rotate your wrist clockwise. In other words, it is not a completely simple maneuver. For example, if the miLoop were delivered above the capsule in the sulcus space and rotated behind the capsule by accident, the consequences would be devastating.
2. There is a huge payoff with the miLoop, as it beautifully cracks even the densest cataracts in halves and quarters. As the loop is retracted into the injector, a dense nucleus will often tilt or prolapse, so it is helpful to have a second instrument in the eye to hold the nucleus down in the bag. In my opinion, the device is not super helpful for soft cataracts, but I do feel it is an absolute game-changer for dense cataracts. It is important to do a good hydrodissection and ensure free nucleus rotation prior to using the device. I do not think the miLoop will replace phacoemulsification, because ultrasound is still needed to remove the dense quadrants, but using the device can significantly reduce phaco energy and effective phaco time by allowing a surgeon to completely bypass the first sculpt and cracking phaco settings and proceed directly to a higher-vacuum quadrant removal setting.
3. I certainly plan on using the miLoop on dense cataracts, especially those in which laser fragmentation is not done. Sculpting with phacoemulsification and cracking extremely dense cataracts are two of the most challenging aspects of cataract surgery, and they are often the source of capsular tears. The device has the potential to greatly reduce this risk. In geographical and demographic pockets where dense rock hard cataracts are prevalent, this device is a must-have.
CONCLUSION
A new strategy may transform the landscape of cataract surgery. Based on my personal experience, the miLoop has the potential to rock the foundation of recent advances and either drastically improve the effectiveness of current technologies or potentially replace seemingly irreplaceable tools.