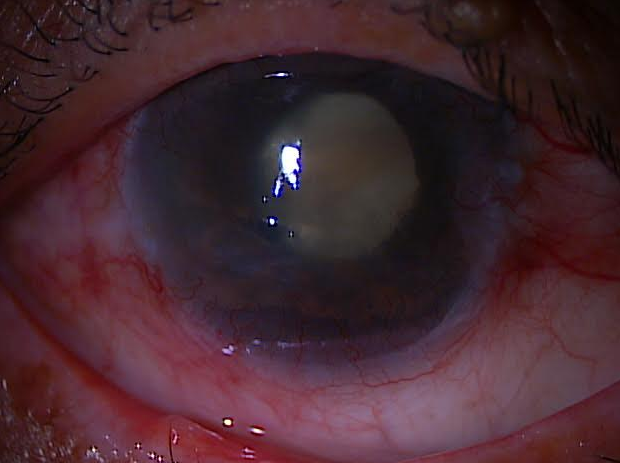
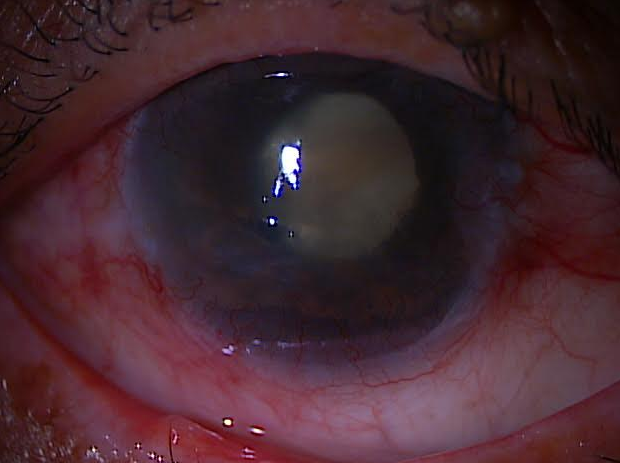
A 78 y ear old patient come in this morning with a eye pressure of 66 mmHg (normal is less than 21 mmHg). He had chronic angle closure glaucoma from a large cataract and narrow angle that was never treated. He has been in a lot of pain for the last year and has no insurance. His son and daughter brought him in. His vision is NLP-No Light Perception.
Since he has no insurance, I am looking for the most cost effective and safe way to take away his pain. Here are the best options:
1. Using eye pressure drops: Timolol is the cheapest but can cause difficulty breathing, asthma, heart beat-issues, depression, as it is a beta blocker. Since he is older, I am trying to avoid this, but it may be the only thing he can affort. Brimonidine (or Alphagan), is also an option but is more expensive. Brand names are usually more expensive.
2. Acetazolamide or Diamox 500mg SR sequels or Diamox 500: can be a good, cheaper option to decrease the pressure and help with the pain.
Most Cost Effective Way to Treat a Blind Painful Eye
Most Cost Effective Way to Treat a Blind Painful Eye
Several options are available for blind, painful eyes that do not respond to topical medications.
3. Retrobulbar injections are a simple and effective alternative: relief is often immediate and usually long lasting, but can cause ptosis (droopy eye) or cosmetic issues in some patients:
a. Inject 2 to 3 mL of anesthetic (such as lidocaine, Carbocaine [Hospira, Lake Forest, IL], or Marcaine [Hospira]; longer acting agents are better),THEN INJECT
b. 1 mL of absolute alcohol, AND THEN
c. additional 1 mL of anesthetic to help ensure that alcohol is not left along the injection tract, which could create a fistula
d. use 25-gauge retrobulbar needle in the traditional retrobulbar space (not peribulbar), injection of the anesthetic, switching the syringe to a second containing alcohol and injecting the alcohol, and then switching back to the anesthetic syringe for the last injection, all through the same needle.
e. Chlorpromazine, 25 mg, has also been used in a similar fashion, with similar reported results.1
Although these injections are uncomfortable, the alcohol much more so than the chlorpromazine, the effects are quick, with a high success rate for complete relief.
Side effects include anesthesia or dysesthesia of the cheek, lid, or brow; injection or marked chemosis of the conjunctiva and lids and face; ptosis; eye movement abnormalities; and potentially a perforated globe
I generally avoid incisional surgery to minimize the interventions on a sightless eye and to minimize the risk of sympathetic ophthalmia in the fellow eye. The most commonly employed options are retrobulbar injection of alcohol or chlorpromazine, cyclodestructive procedures, and enucleation or evisceration.
4. Cyclodestructive procedures, such as laser or cryotherapy to the ciliary body, can be very effective at reducing IOP and are quickly performed with limited need for follow-up, postoperative care, or restrictions compared with other glaucoma surgical procedures.
Complications risk is low but includes:
1. phthisis: where the eye essentially shrinks
2. postoperative pain, which can be significant
3. the possible need for additional treatments because of insufficient effect; and
4. Sympathetic Ophthalmia: very rare, 1 in 1000 or less; I have seen 3 in my career, but because of its potential for harm to the “good” eye, many patients will not choose these procedures.
5. Enucleation and evisceration are often great choices for a blind, painful eye. These procedures have the highest rate of pain relief and a low rate of complications in experienced hands.
Good cosmesis with implants can allow some motility with or without pegs. Be sure to acknowledge the patient and family’s fear of loosing an eye. Many will feel this is a drastic step and may not yet be emotionally or psychologically ready to consider this despite their understanding that their eye will never be able to see again.
Most patients usually prefer to try other means before enucleation, but those who do undergo enucleation are usually among the most satisfied and pleased with the results.
Sandra Lora Cremers, MD, FACS
Notes:
General Issues:
The blind, painful eye presents several challenges for us with respect to its evaluation and management. The first issue in such an eye is to determine the cause of the pain so we can appropriately direct treatment.
1. Blind eyes may have very high intraocular pressures (IOPs) with severe corneal edema but have no pain: treatment may help prevent pain, but there have been no studies to say pressure lowering drops are needed.
2. Sharp spikes of IOP are much more frequently accompanied by discomfort.
3. Paradoxically, some patients who were had no pain before “IOP-lowering procedures” with pressures of 60 mm Hg can begin to have pain postoperatively associated with an acute IOP rebound to 45 to 55 mm Hg.
4. Pain related to IOP is typically described as a dull pain in or around the eye, often similar to a sinus headache, accompanied by pain in the frontal or temporal area.
5. Secondary Corneal Edema, especially microcystic or with bullae, can cause substantial pain: pain is often worse in the morning, presumably because of increased swelling overnight when the eyelids are closed, leading to less drying and oxygenation, and may improve throughout the day.
Treatment options for Secondary Corneal Edema:
a. Topical sodium chloride solutions (5% or 10%) and/or
b. ocular hypotensives to reduce corneal edema
c. bandage contact lenses.
If surgical intervention is planned to reduce the IOP, patients need to understand that some corneal swelling and related pain may not be resolved even at low IOPs.
Pain related to high IOPs may also respond to topical ocular hypotensive medications, and this is where therapy usually begins unless these are poorly tolerated or too costly. Chronically painful eyes, with or without elevated IOPs, may respond to topical steroids and cycloplegics such as atropine, which presumably exert their effect by reducing the inflammatory component and any ciliary spasm. These agents are more likely to be effective in patients who are photophobic when their other (seeing) eye is exposed to light.
References
J Pak Med Assoc. 2015 Jun;65(6):678-80.
Ann Ophthalmol. 1990 Dec;22(12):460-2.
1. Chen TC, Ahn Yuen SJ, Sangalang MA, Fernando RE, Leuenberger EU. Retrobulbar chlorpromazine injections for the management of blind and seeing painful eyes. J Glaucoma. 2002;11:209-213.
2. Kahook MY. In which glaucoma patients should I consider cyclodestruction? In: Heuer DK, Gedde SJ, Lewis RA, eds. Curbside Consultation in Glaucoma: 49 Clinical Questions. Thorofare, NJ: SLACK Incorporated; 2008.
3. Sabates R. Choroiditis compatible with the histopathologic diagnosis of sympathetic ophthalmia following cyclocryotherapy of neovascular glaucoma. Ophthalmic Surg. 1988;19:176-182.
4. Edward DP, Brown SV, Higginbotham E, Jennings T, Tessler HH, Tso MO. Sympathetic ophthalmia following neodymium:YAG cyclotherapy. Ophthalmic Surg. 1989;20:544-546.
5. Shields CL, Shields JA, De Potter P, Singh AD. Problems with

