Myofascial pain syndrome is a chronic pain disorder that can be very frustrating for patients and physicians alike. In myofascial pain syndrome, pressure on sensitive points in your muscles (trigger points) causes pain in seemingly unrelated parts of your body, which is called referred pain.
Myofascial pain syndrome typically occurs after a muscle has been contracted repetitively. This can be caused by repetitive motions used in jobs or hobbies or by stress-related muscle tension.
1. Massaging: by hand or with electric massager you can buy for cheap on Amazon
3. Physical therapy
4. Trigger point injections.
5. Acupuncture
6. Pain medications and relaxation techniques also can help: but avoid pain meds that become addictive.
7. A recent patient told me about a specialist in this area below: Dr. Michael T. Singer
Science behind Acupuncture:
Does Acupuncture and Massaging Work?
The short answer is yes.
But it is very interesting as to why it works.
For years, the science community was skeptical about such treatments: do they really worked with pain or is it a placebo effect.
Now we know they do work with pain and other conditions, and more is understood on why it works.
See below.
First the pizoelectricity of the body is an important part of feeling normal and not having pain. These crytals in the pineal gland of the body show pizoelectricity.
Calcite microcrystals in the pineal gland of the human brain: first physical and chemical studies.
Abstract
A new form of biomineralization has been studied in the pineal gland of the human brain. It consists of small crystals that are less than 20 microm in length and that are completely distinct from the often observed mulberry-type hydroxyapatite concretions. A special procedure was developed for isolation of the crystals from the organic matter in the pineal gland. Cubic, hexagonal, and cylindrical morphologies have been identified using scanning electron microscopy. The crystal edges were sharp whereas their surfaces were very rough. Energy dispersive spectroscopy showed that the crystals contained only the elements calcium, carbon, and oxygen. Selected area electron diffraction and near infrared Raman spectroscopy established that the crystals were calcite. With the exception of the otoconia structure of the inner ear, this is the only known nonpathological occurrence of calcite in the human body. The calcite microcrystals are probably responsible for the previously observed second harmonic generation in pineal tissue sections. The complex texture structure of the microcrystals may lead to crystallographic symmetry breaking and possible piezoelectricity, as is the case with otoconia. It is believed that the presence of two different crystalline compounds in the pineal gland is biologically significant, suggesting two entirely different mechanisms of formation and biological functions. Studies directed toward the elucidation of the formation and functions, and possible nonthermal interaction with external electromagnetic fields are currently in progress.
Second, the fascial plane (the tissue wrapping all the muscles of the body show pizoelectricity.
Acupuncture and massaging directly stimulate the fascial plane.
Basic science is trying to find out exactly how acupunture helps pain issues on the molecular issue.
For one, I know that if I massage certain pressure points on my shoulders around the trapezius muscle when I feel I am getting a cold or flu, I can avoid getting sick (if I also take a Cold Eeze zinc lozenge. I have noticed the same for my kids: if I massage the trapezius muscle in certain areas so it hurts (I and they feel abnormal pain in this area when getting sick which usually is not painful), I can help them decrease the days they are sick or avoid the cold. I have also bogged about the pressure points I use on myself and my kids to get rid of a headache: the trapezius muscle area, the neck muscles, and the superior orbital notch (and drinking alot of water): works every time. Is it the extra water I make the kids or myself drink or the massaging, I do not know: likely both. But it works for us and we never use pain meds for headaches.
I hate “non-scientific” 1 person case reports. But since it has been years not that I have been noticing this and now I see it helping my family, I will briefly mention it here. I have become a believer in the pizoelectric properties of the fascial planes around muscles and the ability to stimultate these planes to avoid and remove pain in other parts of the body and even help attack viruses (that is a big jump, scientifically, I know.)
Sandra Lora Cremers, MD, FACS
Published online 2011 Dec 31.
Fascia Research from a Clinician/Scientist’s Perspective
Abstract
The upcoming Third International Fascia Research Congress will have much exciting information for the clinician, as well as for the clinical and basic science researcher. This paper provides a perspective from a clinician/scientist, including the fascial network of body-wide connections between and within individual cells, and sharing of loads between muscle and fascia. Basic studies of fibroblast cell shape show the impact of manual therapy, acupuncture, and yoga-like stretching at the cellular level. Advances in scientific equipment have made it possible to study a layer of hyaluronan fluid, which allows sliding between deep fascia and muscle. Collagen fibers within fascia affect both blood flow to muscles and lymphatic fluid flow.
Keywords: fascia, conference, tensegrity, fibroblast, fluid flow, collagen
INTRODUCTION
Fascia research. What is all the buzz about? Why is there yet another international fascia congress in Vancouver, March 28–30, 2012, and why should we manual therapists attend? (Yes, I mean “we”). I am a physician in physical medicine and researcher who is crazy enough about research to have obtained my PhD during my residency program. As my wife will verify, I live, breathe, and dream research and, according to my mother, at age three I stood still for 45 minutes in the warmth of the winter sunlight streaming in through our dining room window, holding a jar of honey, proclaiming “I doing exerment [experiment]”. The budding scientist in me was studying changes in the viscosity of a fluid with application of heat. I am still doing much the same thing 60 years later. However, I also am a manual therapist with a half-time clinical practice as a Certified Advanced Rolfer™.
I experienced Rolfing® Structural Integration in 1970, before attending medical school, and have carried the perspective on fascia developed by Dr Rolf throughout my career. Thirty years ago, I studied the clinical practice and scientific basis of muscle strengthening, exercise, stretching, heat, and other therapeutic modalities that are still used in my medical specialty today. Then our resident didactic lectures got to connective tissues. From the research standpoint, all we knew was that, if you heated a rat tail, you could stretch it. I eagerly absorbed the clinical experience of my teachers, learning procedures for dealing with connective tissues developed during the polio era; but my body knew there was more.
Fast-forward 20 years. As director of Research at Kessler Institute for Rehabilitation in New Jersey, I earned the trust of the hospital leaders, who were confident that I knew my material thoroughly and well, even though they also recognized that they had no real hope of understanding it. From that vantage point, I convinced them to sponsor a training program in structural integration at the hospital in 1991, for myself and other physical therapists. The therapists began using these techniques with the traditional rehabilitation patients with good results – even publishing them
(1). I stayed in my research tower, except to use my bodywork training when faced with the challenge of getting Christopher Reeve off his ventilator (you can see some details in his remake of the Hitchcock thriller
Rear Window). Even becoming a professor at UMDNJ School of Osteopathic Medicine did not dislodge me from my research perch. When I had the opportunity in 2000 for a sabbatical from my academic position, however, I did not write a book or do a new research project or visit a research laboratory. I chose to expand my horizons by setting up a clinical practice as a bodywork practitioner, and have maintained a half-time practice as an Advanced Rolfer ever since. In this editorial, I will join the ranks of my fellow manual therapy practitioners and give you my clinical perspective on the upcoming fascia research congress.
DISCUSSION
The fields of acupuncture, massage, structural integration, chiropractic, and osteopathy all present clinical hypotheses with fascia as a central theme. Yet many practitioners are unaware of the scientific basis for evaluating such hypotheses, and few know of the sophistication of current laboratory research equipment and methods. I will fill in some of these details, to give a flavor of what to expect at the next fascia congress. The hallmark of the fascia congress is interaction between clinicians and scientists, which is reflected in its theme: Fascia Research–What Do we Notice and What Do we Know—continuing the clinician–scientist dialogue. Particular effort is being made to incorporate clinical translation immediately following scientific presentations, and vice versa. We planned for time after each keynote to do this in Amsterdam in 2009, but then we received some incredibly exciting abstracts which were given those time slots instead. That was one reason, among many, to choose the Massage Therapists’ Association of British Columbia to be the host—to make sure the science is translated into relevant concepts for the clinician.
I publicly admit that I was overwhelmed by the first congress, and similarly by the second. Both my clinical side and my research side had difficulty digesting all the material, so I watched the DVD recordings again, and again, and again. To be generous, I now understand perhaps half of what was presented. I went through probably 2000 recent papers on fascia to select a few outstanding ones for the 2012 program book, and it took me two hours to really understand one diagram from one paper selected—and this was after I had already used that diagram in a summary talk I gave on fascia research. The good news for you, my readers, is that I can now explain this material to you in ways that make sense to my clinical half. This editorial comes out of a four-hour workshop I recently gave at the AMTA national convention.
It’s All Connected
We all know the children’s song “the hip bone’s connected to the thigh bone …”. Anatomy texts show these bony connections and two joint muscles such as the gastrocnemius, but they don’t show the whole picture. I have a simple clinical demonstration of fascial continuity extending from the occiput to the calcaneus that I show medical students. It is quite simple. Sit in your chair with your knees bent and dorsiflex your ankle. Now stand up and do the same thing. It does not move as far—and we know why. The gastrocnemius extends across both the ankle and the knee. Now take that leg and with the knee straight, put it on the table in front of you. The foot moves less. Now bend your trunk forward. Even less motion. Next, drop your head. Now you can really feel tightness in your calf. This demonstrates just one simple fascial connection, the back-line, but the fascial connections throughout the body are far, far more intricate.
We find that muscles hardly ever transmit their full force directly via tendons into the skeleton, as is usually suggested by our textbook drawings. Rather, they distribute a large portion of their contractile forces onto fascial sheets. In some muscles (for example the Gluteus maximus), 85% of the fibers go to the distal fascia (in this case the Fascia lata) rather than to the theoretical muscle insertion. Muscles also transmit forces laterally to neighboring muscles; in some cases (measured in the rat leg), almost 50% of the muscle-generated force goes laterally rather than to the muscle tendon
(2). These forces go to synergistic partners, as well as cross the limb to antagonistic muscles. Thereby they stiffen not only the respective joint, but may even affect regions several joints away. The simple questions from musculoskeletal textbooks regarding “which muscles” are participating in a particular movement cannot be simply answered. Muscles are not separate individual functional units, no matter how much the textbook authors and your anatomy instructors want them to be. Rather, most motions are generated by many individual motor units, which are distributed over some portions of one muscle, plus other portions of other muscles. The tensional forces of these motor units are then transmitted to a complex network that converts them into the final body movement. While these pathways have been studied in the extremities where muscles cross one or two joints, there is little information on whether the same principles apply in the trunk, as well. However, the next fascia congress will show anatomic pictures of minute fascial strands between muscles in the neck which may well be myofascial connections. The program book for the 2009 congress shows tiny fibers extending from the muscle to pull open the nitric oxide receptors on the arterioles and, thus, immediately increase blood flow to that muscle
(3).
It rapidly gets very complicated. There are nerves in the motor cortex of the brain which directly communicate with muscles via a single synapse in the spinal cord. Fortunately, we do not have to use these often, or we would spend forever figuring out how to move. We have patterns of movement which we are born with, and others which we learn through repetition, and we generally rely on these automatic patterns to accomplish our daily activities. Remember how many months it took you to learn how to walk the first time? You may not, but your parents do. And we don’t ordinarily forget these patterns, even after many years of disuse. How many of us have forgotten how to ride a bicycle? If you have a stroke which interferes with movement patterns, learning to walk the second time around goes quicker.
Many years of scientific studies have begun to probe the nature of movement, and the last fascia congress was held in a school of movement science. The individual motor units used for a particular movement depends on the force required—if more force is required, motor units with larger numbers of muscle fibers are used. If the motion requires less force, smaller units are used. Furthermore, there is a rotational system so that the motor units you use at any particular moment in time get a brief rest and other ones of similar size take over briefly
(4). Similarly, if you encounter unexpected resistance part way through performing a motion, more motor units are automatically brought to bear. This “sharing the load” function happens without our conscious awareness.
At the 2007 Fascia Research Congress in Boston, Dr Gracovetsky showed us that in the lumbar spine the load is shared between muscles and fascia
(5). If the load were always on the muscles, they would fatigue; if it were always on the fascia, they would stretch out. Moving back and forth between the two allows the body to make use of the best characteristics of both. We find that fascial stiffness and elasticity also play a significant role in many ballistic movements of the human body. How far you can throw a stone, how high you can jump, and how long you can run depend not only on the contraction of your muscle fibers, but also to a large degree on how well the elastic recoil properties of your fascial network are supporting these movements. This is graphically illustrated by the double-amputee Oscar Pistorius, whose entrance into the 2008 summer Olympics was blocked because it was thought that his spring-like artificial legs gave him an unfair advantage over able bodied runners. It turns out they didn’t—fascia is even better!
We are not just talking about fascial connections between muscles, bones, ligaments, and other large body structures. These fascial connections reach to the very interior of the cell, all the way to the nucleus. The scientific progress in documenting these connections has been truly amazing. As lead speaker in 2007, Dr Ingber showed us how the slightest touch on a cell surface with a micropipette caused the nucleus to immediately expand and begin DNA transcription
(6). The older models of the cell regarded it as a formless water balloon. Dr Ingber showed that, instead, the cell is built more like a tent with poles bearing compression and guy wires under tension, following the principles of tensegrity. He showed us that the microtubules in the cell are the equivalent of the tent poles, and the actomyosin filaments are the guy wires. The living cell is a mechanical structure with a force balance between compression-bearing microtubules and tension-bearing bundles of actomyosin filaments. The tent pegs are the integrin receptors. The cells are anchored to the extracellular matrix by clusters of integrin receptors, which connect extracellular proteins and filaments to intracellular filaments, the actin-associated molecules. These integrin receptors also serve to sense physical forces outside the cell and transmit that information through mechanical connections throughout the cell to the nucleus, as well as to multiple locations in the cell. This cytoskeleton provides both mechanical structure and direction to biochemical reactions within the cell. The cell can thus convert external mechanical signals into internal biochemical reactions
(7). In a similar fashion, development of the embryo is strongly influenced by the mechanical environment of the cell and is guided by this extra- and intracellular fascial network
(8).
Use of the experimental methods recently developed may allow us to explore the effects of externally applied forces that create repetitive stress disorders or assist in manually applied therapies. Many clinical therapies use externally applied forces based on empirical observations (some ancient), but rarely if ever are these treatments anchored in the biomechanical environment of the cell. Recent developments in medical diagnostic imaging may allow direct observation of this biomechanical context.
Dr Frederick Grinnell is doing some very important work at the cellular level, yet when he was invited to be a keynote speaker at the 2007 fascia congress he did not understand why his work was so important, despite his receiving Rolfing bodywork for many years. I had to explain the potential clinical meaning of his science and then he enthusiastically agreed. If we remain at the cellular level for a moment, we can look at the primary cell in fascia, the fibroblast. We find that fibroblasts synthesize, organize, and remodel collagen, depending on the tension between the cell and the extracellular matrix. In the 2007 Fascia Congress, Dr Grinnell showed so elegantly that at low tension from outside the cell, the fibroblast is in a resting state with low synthesis of collagen matrix
(9). When placed in a high tension matrix the fibroblasts increase their collagen synthesis and cell proliferation. The fibroblasts appear quite different in these two states. In low tension, they have a small cell body with dendritic extensions connected to other cells by gap junctions. In high tension matrix, the fibroblasts assume a larger cell body of lamellar shape. An individual fibroblast can change back and forth between these two cell morphologies. By looking in the microscope at the fibroblast, from the size of the cell body one can infer the tension placed on the cell: the higher the tension, the larger the cell body. This change in cell body size affords the opportunity for measuring at the cellular level the effects of therapies designed to change fascial tension.
Each fibroblast can remodel nearby collagen matrix, and this local remodeling can spread throughout the matrix to result in large scale matrix contraction. By exerting traction on the matrix, the fibroblast can either cause motion of the collagen or movement of the fibroblast through the matrix
(10). Fibroblasts produce and degrade matrix proteins, with an indirect effect on matrix stiffness. They can also differentiate into myofibroblasts, which can contract and increase matrix tension. By changing shape, the fibroblast can affect stiffness and viscosity of connective tissue within minutes, consistent with the mechanotransduction model of microtubule network expansion and actomyosin generated tension proposed by Ingber
(7). The fibroblast may also remodel cell matrix contacts in the direction of tissue stretch to reduce tension
(11). Does the fibroblast just respond to the mechanical forces around it, or is it a primary force for directing growth and adaptation? Either way, it is a key player in the fascial orchestra, and perhaps it is the conductor.
And Therapies Actually Do Something
Using these new techniques for imaging the fibroblast, at the first congress in 2007 Drs Standley
(12) and Langevin
(13) showed the cellular effects of manual therapy, acupuncture, and yoga-like stretching. And they continued with new findings from their research, which they presented at the second Fascia Congress in Amsterdam in 2009
(14,15). Connective tissue actively regulates matrix tension in response to stretch as a normal, dynamic physiological process. Understanding how cells respond to forces can lead to potential new treatments and refinements on existing ones.
And there’s more . . . several new areas will be presented in the 2012 fascia congress. Some of this research is not new, it is more than ten years old, yet we are just appreciating its application.
The deep fascia is a highly vascular structure with a superficial and a deep layer, each with an independent rich vascular network of capillaries, venules, arterioles, and lymphatic channels. The presence of mast cells in deep fascia suggests a protective role similar to other connective tissues. The deep layer has few elastin fibers but does have myofibroblasts, suggesting contractile ability. Any active contraction would need to be controlled by a nerve supply and, indeed, one finds myelinated and unmyelinated nerve axons and Schwann cells in these deep fascial layers. The deep fascia is not just a tough barrier structure of collagen and elastin, but is a metabolically active vascular layer which provides gliding and protective functions
(16). Deep fascia has parallel longitudinal collagen bundles and rudimentary elastic laminae, giving it both high tensile strength and elasticity. At the junction between the deep fascia and the muscle, without any special secretory cells, the fascia is able to maintain a lubricating layer of hyaluronic acid (hyaluronan) which, like a hydraulic fluid, allows sliding between the fascia and neighboring muscle. However, when the epimysium is disrupted in surgery, overlying fascia does not remain distinct and does not create a gliding layer over the scar
(17). More recent findings show that while hyaluronic acid is a lubricant, breakdown products of this large molecule are themselves tissue irritants
(18), and fragments from collagen, elastin, and laminins in the extracellular matrix also modulate activities of inflammatory cells
(19).
This layer of hyaluronan is 100–200 microns thick. The architecture of the fascia allows continuity of nerves, blood, and lymph vessels between the sliding tissues. With trauma to the muscle, the overlying fascia no longer produces the sliding layer of hyaluronan. Restoring this natural sliding mechanism becomes the next task for the manual therapist.
I was a car mechanic before I went to medical school, and learned that my hands could detect valve clearances with an accuracy of one thousandth of an inch (that equals 25 microns). I would lie on my back, reach up around the engine on the old air-cooled VWs, pop off the valve cover, and wiggle the rocker arm to check the valve clearances. From time to time, I would go through the effort of squeezing in a feeler gauge to check what my fingers were telling me. To put this in perspective, a red blood cell is 8 microns in diameter and a sheet of paper is about 75 microns. Most of us can tell the difference between 75 and 150 microns, for example when we turn the page on a magazine and accidentally get two at a time. I am convinced that feedback from the clinician’s hands can guide manual therapy, although we don’t yet have the bodywork equivalent of the mechanics feeler gauge to check our perceptions. The newer musculoskeletal ultrasound imaging machines are beginning to have sufficient resolution to see a hyaluronic acid layer of 100–200 microns (MRI resolution is about 300 microns). I have tested the ultrasound machine I use in my clinical practice. It can measure thickness with an accuracy of almost 50 microns in my research projects when I insert objects into mozzarella cheese, but I can’t consistently see the hyaluronic acid layer in humans yet. My hands are still better.
References:
1. Dr. Michael T. Singer is a board-certified Diplomate of the American Board of Prosthodontics (1983) and the American Board of Orofacial Pain (1996). Dr. Singer is board certified in the specialties of Prosthetic Dentistry, and Orofacial and Maxillofacial Prosthodontics; his practice specializes in the treatment of the full range of facial and oral pain disorders and in the restoration of facial structures lost to cancer, trauma, and birth defects. He has over 30 years of clinical experience treating patients and consulting in a broad range of interdisciplinary cases.
Dr. Singer graduated from Northwestern University Dental School in 1974 as well as the Walter Reed Army Medical Center Prosthetic program. He is also a graduate of the Bethesda Naval Dental School program in Maxillofacial Prosthodontics and the University of Minnesota Orofacial Pain graduate program. He subsequently served in the Army at Walter Reed Army Medical Center in Washington, D.C. During his career there, he became a highly trained officer in the United States Army Dental Corps, completing 4 residency programs in 6 years of postdoctoral study:
- General Dentistry Residency
- Prosthodontic Residency
- Maxillofacial Prosthodontics Residency
- Orofacial Pain Residency
At Walter Reed, Dr. Singer was Chief of the Orofacial Pain and the Maxillofacial Prosthodontics Clinic. He retired from the Army and Walter Reed Army Medical Center in 1997 with the rank of Colonel.
Dr. Singer entered private practice in 1997. He also holds a position as a Clinical Instructor in the Advanced Prosthodontics Program at the University of Maryland Dental School, where he has taught since 1997.
Dr. Singer provides prosthetic restoration to patients with an advanced and/or complex temporomandibular disorder as well as to those with a severely compromised dentition. Clinically, his special interests include prosthodontics, maxillofacial prosthodontics, and orofacial pain.
A member of the faculty of the University of Maryland Dental School graduate department of Prosthodontics, Dr. Singer has lectured to dentists and physicians across the United States. He is a featured speaker for the American Academy of Pain Management.
http://www.michaelsingerdds.com/about_michael_singer.html
2. This is controversial but very interesting. While I do not believe at all that wearing any crystals help with anything: have never seen any worthwhile study to indicate they help, the pineal gland does have very interesting properties that need to be explored more.
https://physics.knoji.com/the-piezoelectric-effect-and-the-pineal-gland-in-the-human-brain/
The Piezoelectric Effect and the Pineal Gland in the Human Brain
Learn how electromagnetic energy affects the Pineal Gland in the human body and how the Calcite Micro-crystals respond and reproduce electromagnetic energy.
As we explored the Piezoelectric effect through my other article pertaining to Quartz Crystal in which we described the Piezoelectric effect as electricity resulting from pressure, which holds an accumulated electric charge as a solid material, in this article we are going to further explore how this effect pertains to the Pineal Gland inside the human brain.
In this article we will be exploring how the Piezoelectric effect relates to the human brain and electromagnetic energies within and outside the human body that pertain to extra sensory perception and energetic sensitivity, especially during exercises that focus on enhancing the electromagnetic response through meditation, dreams and environmental stimulation. In metaphysical literature, the Pineal Gland has been described as the “seat of the soul”, the “third eye”, and “Brow Chakra (Ajna Chakra). The reference to being the “third eye” is quite ironic considering the anatomy of the Pineal Gland has a lens, cornea and retina as does the actual eye.
Physiologically, the Pineal Gland is a pine cone shaped gland of the endocrine system that is approximately the size of a raisin, and is responsible for producing Melatonin which influences sexual development and regulates the sleep cycles in the human brain and body. More specifically, the Pineal gland is responsible for converting Serotonin into Melatonin and is the only gland in the body that does so. It is the first distinguishable gland present in the brain and is recognizable within three weeks gestation of fetal development.
Image Source
Inside the Pineal Gland are Calcite Micro Crystals consisting of Calcium, Carbon and Oxygen that produce bioluminescense; a “cold” light that produces light without heat, ranging in the blue-green light spectrum. In deep sea marine life that uses bioluminescense in the same way, we can look forward to more emphasis on developing the Pineal Gland for transparency within the cellular tissue of the human body. For example, there have been ongoing studies in labs with animals such as rats in which bioluminescent imaging is able to detect cancer or abnormal cell growth in comparison with thermal imaging that makes the study and conclusions more efficient and precise.
Image Source
The Calcite Micro-crystals are said to have their own Piezoelectric effect that is responsive to electromagnetic energies outside the physical body, and can also produce it’s own electromagnetic energy. A new form of bio-mineralization has been studied in the human Pineal Gland using scanning electron microscopy and energy dispersive spectroscopy.
A study conducted in Israel by the Department of Chemical Engineering through the Ben-Gurion University of the Negev in Sheva, these tiny micro-crystals were noted to have a texture that may be noncentrosymmetric because of the structural organization of the sub-unit, even though the single crystals do have a center of symmetry which gives one reason in which the crystals are considered Piezoelectric, similar to the calcite crystals inside the inner ear. Among many results, it is discovered that the calcite micro-crystals would have piezoelectric properties with excitability in the frequency range of mobile communications which brings into question the entire spectrum of energy waves we encounter every day that could, in the long term, create morphological change on cellular membranes of related cells.
What this means is that any energies that produce an electromagnetic response in relation to the Pineal gland could alter energy patterns within the body and brain from the central nervous system to sexual function, sleep cycles or sleep deprivation and hypersensitivity to electromagnetic stimulation through one’s environment.
Image Source
Discovering the alteration that electromagnetic frequency waves of energy has on the Pineal Gland is not new to science, Metaphysicians or spiritualists.
According to author Preston B. Nichols who wrote The Montauk Project copyright © 1992, states that in the 1960’s, military personnel of the Air Force were working on the Sage Radar project on a decommissioned base, Montauk. It was reported that by changing the pulse duration and frequency of the radar that used a middle infrared band of energy waves, they could change the general mood of the people on the base.
Results of stronger pulses of infrared energy waves on the brain, and especially the Calcite Micro-crystals in the Pineal Gland are:
- Sleepiness
- Crying
- Agitation
- Depression
- Anxiety
- Aggression
- Fear
- Terror
- Hopelessness
- Grief
- Apathy
- And even Death
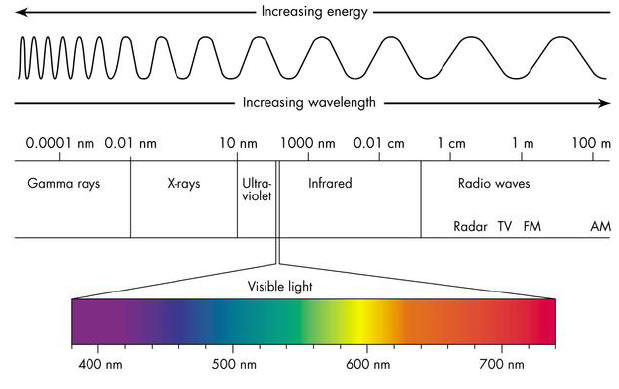
Infrared energy waves are the lower frequency waves on the light spectrum. Low frequency waves have a longer wave length which correspond with lower emotional energies and moods. While higher frequency waves such as those in the green, blue and violet range produce higher emotional energies and moods.
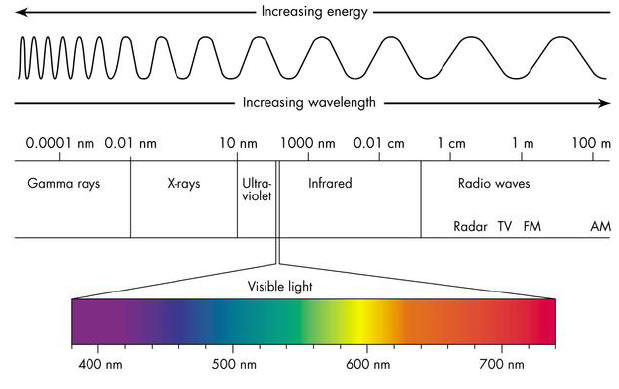
Image Source
The same results can be seen in sound waves as well. A great study for comparison is Dr. Masaru Emoto in his groundbreaking research of how human consciousness can intentionally and unintentionally effect the molecular structure of water, as well as studying the result of sound wave vibrations. For example, research has been done in which large metal plates are subjected to a range of different sound waves that affect grains of sand sitting on top of the metal plate. The conclusion is that the grains of sand develop and shift into geometric patterns and shapes depending on the sound waves that are applied.
Image Source
Metaphysically, quartz crystals resonate very closely with the Piezoelectric effect that the Calcite Micro-crystals produce within the Pineal Gland as well as inner ear, which makes them highly effective for the usage of spiritual endeavors, meditation, altering one’s mood or altering one’s state of well being that range in subtlety or intensity for the individual using crystals as a form of energetic therapy.
Similar to how the lower infrared band of frequency waves can adversely affect the mood and health of the human body, so can the higher frequency waves that can positively affect the mood and health of the human body.
Avoiding geographical areas or electronic equipment that emit large quantities of infrared energy waves supports a more positive experience in relation to the Pineal Gland and assists in keeping in balance the moods, sleep cycles and sexual health of the person.