Patients that have “Pain without Stain” or “Neuropathic Dry Eye” are often our toughest patients to help. Patients remain frustrated as most standard dry eye remedies do not relieve all the pain or do nothing to help. Doctors/surgeons/doctors remain frustrated as all their recommendations and treatments do not fully heal the patient. Many eye surgeons have given up on even seeing these patients for this reason.
A colleague noted recently that the temptation for eye surgeons is to limit one’s practice to only surgical patients and “not waste chair-time” by these “impossible to treat patients.” Unfortunately many eye surgeons have this sentiment.
Many of these patients have tried all standard options provide. These patients come to see me usually having tried multiple options with no relief and having seen many eye doctors and surgeons on the way to see me. Some of these patients are helped significantly with Intense Pulse Light and Meibomian Gland Probing/Expression with or without Autologous Serum, PRP, and (we await results for Stem Cell injections). Some of them have not been helped with even these procedures.
What is the cause of Neuropathic Eye Pain/Neuropathic Dry Eye?
Neuropathic pain/ Neuropathic Dry eye is due to a combination of many factors. Chronic inflammation is a key component. There are many factors that can contribute to chronic, microscopic inflammation at the nerve cell level.
Prolonged ocular surface stimulation can alter neurons and lead to pain amplification expressed chonic eye pain. My concern is that the chronic stimulation of looking at electronic screens is a big factor that is taking many patients over the edge. Other negative factors that cause chronic microscopic inflammation are previous isotretinoin/Accutane use, LASIK/PRK, chronic allergy, ocular rosacea, oral contraceptives use [Recently a patient told me a world renowned Harvard eye surgeon told her that her Mirena IUD caused her Sjogren’s syndrome: more on that in an upcoming post], smoking, previous eye trauma, autoimmune disease (like Sjogren’s syndrome, Rheumatoid Arthritis, Lupus), previous chemotherapy, radiation, Bells Palsy, Stevens Johnson Syndrome, Graft Versus host disease. Also general aging and hormonal changes can cause nerve fiber irregularities which can also exacerbate chronic eye pain symptoms.
Many patients with Neuropathic pain/ Neuropathic Dry eye also have other disorders that central pain processing, such as depression, anxiety, and insomnia. (Reference 2, 3)
Inflammation begins on the ocular surface with chronic stimulants leading to chronic inflammatory cytokines release. This can lead to increased activity of sensory nerves or chronic sensory nerve firing. Over time, chronic microscopic inflammation can lead to peripheral sensitization which means the corneal nerves become “numb” to the stimulus and continue to fire even without stimuli or irritants.
As Dr. Anat Galor notes in her paper below (Reference 1):
Increased activity of sensory nerves can also cause inflammation in the form of neuro-inflammation, which in turn ramps up the activity of pain-carrying nerves, leading to a self-perpetuating phenomenon known as peripheral sensitization.7 For many patients this can be reversed after resolution of the inciting stress and ocular surface inflammation.8 Some dry-eye patients experience only transient episodes of pain, whereas others have persistent symptoms of chronic disease.
Neuropathic pain is by definition “pain arising as direct consequence of a lesion or disease affecting the somatosensory system,” and is often chronic.9
The transmission of dry-eye pain signals to the somatosensory cortex is not a passive process. Along the way, these electrical signals are modified by feed-forward and feedback systems that typically intensify the signals. This explains the unique property of pain to become amplified during a constant noxious stimulus, in contrast to most other types of sensory responses that adapt during persistent stimulation and thereby attenuate the responses. This physiological phenomenon, known as central sensitization, occurs with dry eye-like pain as well.8 Since the trigeminal brainstem was shown in animal models to be the location of central control of homeostatic corneal wetness,10 corneal algesia11 and aversive responses to light,12 the brainstem may also be the origin of the clinical expression of dry-eye-related pain. The possibility that disorders of the dry-eye alarm system itself can explain the variety of clinical patterns associated with dry eye-like pain offers a strikingly different perspective. Moreover, the location and persistence of this dysfunctional alarm system can alter the functional anatomy through the well-known, innately powerful neuroplasticity of the central nervous system. These maladaptive changes in the CNS result in neuropathic pain.
Possible Origins of the Pain
For us to be able to manage these cases effectively, it’s important to recognize the factors influencing neuropathic pain. Age-related dry-eye disease is characterized by the attrition of corneal nerve fibers. Its consequences are associated with an increased sensitivity to tear evaporation, or corneal evaporative hyperalgesia. Pain fiber attrition also occurs in de-afferentation hypersensitivity, a phenomenon found in the skin of healthy elderly subjects. The loss of nerve fibers in these conditions is associated with increased activity of the surviving nerves.13 The parallels between this condition and age-related dry eye are striking.
In mice, it has been demonstrated that sensory nerve injuries, such as those caused by LASIK axotomies, trigger a phenotypic change in the somata of the surviving nerves from conduction to regeneration, promoting the expression of atopic pain generators that are hypersensitive and hyper-responsive14 and that are transported to the regenerating nerve sprouts and the central terminals of severed axons from the nerve somata in the trigeminal ganglion where they’re expressed. This likely is responsible for the complaints of dry-eye symptoms following refractive procedures. Persistence of the regenerating phenotype long after healing has occurred, sometimes years after LASIK, as suggested by the characteristic morphology of regenerating nerves and increased numbers of mature dendritic cells in the sub-basal plexus, may explain the chronicity of dry-eye pain even in the absence of external signs of inflammation.
Both nociceptive and neuropathic mechanisms likely play a role in chronic itch and DE. Nociceptive pain (defined as pain that arises from actual or threatened damage to non-neural tissue and is due to the activation of nociceptors46) is driven by chronic ocular surface abnormalities that are seen in many DE sub-types (pSS, graft versus host disease). With time, inflammation, trauma, and chronic activation of nociceptors can lead to permanent changes in nociceptor structure and function (i.e. sensitization) that can occur both peripherally and/or centrally, thus adding a neuropathic component to the pain (defined as a pain due to a lesion or disease of the somatosensory system46).”
Thus there are patients who have tried many of the standard options but still have chronic pain.
It is very frustrating to not be able to provide comfort to a suffering patient.
More and more of my severe dry eye patients are trying these oral drugs below.
Most, unfortunately have not helped or the patient could not tolerate the side effects, but some cannot live without them.
Why do some patients get better with these pills and others do not? No one knows for sure, but in some patients it is worth a try if all else has been tried.
How do you tell if you have neuropathic pain?
Here are some ways we can tell the eye pain is Neuropathic:
1. The eye pain remains the same after the installation of anesthetic. Those patients without neuropathic pain get relief of their pain usually.
2. There are no real objective signs of dry eye on the cornea or minimal meibomian glands atrophy.
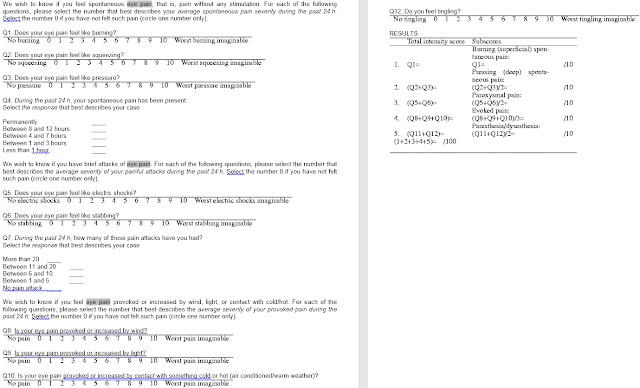
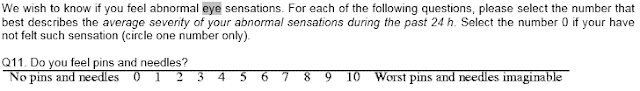
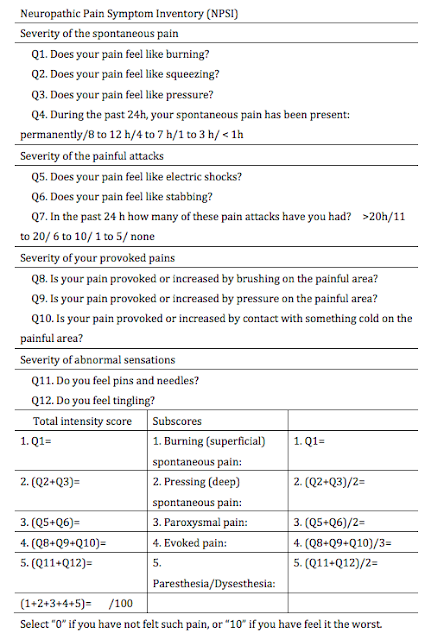
3. Take the Neuropathic Pain Symptom Inventory.
Dr. Anat Galor adds in these questions: See below
a. Do your eyes feel hot and burning?
b. Are you sensitivity to light?
c. Are you sensitivity to wind?
Dr. Anat Galor’s Version of Neuropathic Pain Symptom Inventory (NPSI): from reference 1 below & posted here with her permission.
“The NPSI has been validated as a self-report instrument for assessing neuropathic pain,20 has been used to quantify different aspects of neuropathic pain,20 and has been found to correlate with mechanical and/or thermal allodynia and hyperalgesia assessed using Quantitative Sensory Testing (QST).21“
Original
How to Treat Neuropathic Eye Pain?
1. First try all the standard options for dry eye pain: Lid hygiene, warm/hot compresses with lid massaging, blinking exercises, frequent blinking, long-paused blinking, voiding electronic screen use as much as possible (also take breaks every 10min for 10 sec, look 10f away), clean eyelids with diluted tea tree oil and/or Avenova or hydrochor; use only non-preserved artificial tears (Retaine or Omega rich tears), Eat Omega 3 2000-4000mg/day; stay on an anti-inflammatory diet until we can get the pain to go away (ie, gluten free, Paleo recommended); Use Doxycyline 20mg/day if able to tolerate and/or have ocular rosacea as a contributing cause.
Get meibography and have it scored.
2. If these do not help and you have enough oil glands on meibography, try Lipiflow at least 2x over a 6-10 month period (this is the only Dry Eye procedure approved by the FDA to save meibomian glands but only 70% or so of patients get relief of dry eye symptoms).
3. If no improvement: try IPL if you are a candidate with videotaped expression x 4-6 (if skin type allows this) to see if this helps.
4. If still no improvement, try Autologous Serum (AS), or Platelet rich plasma (PRP) eye drops. Amniotic drops have come out but no publications yet say it helps unlike AS, PRP to my knowledge.
5. Meibomian Gland Probing and Expression first alone and then with Autologous Serum (AS), or Platelet rich plasma (PRP) if AS did not help has helped many patients with Neuropathic Eye Pain but it is not 100%. Studies into the use of autologous Stem Cell injections into the meibomian glands, lacrimal glands, subconjunctival, and intravenous have been started but no publications have shown they work yet. All these treatments in #5 are experimental and not FDA approved.
6. Try also Prokera/Amniotic membrane to see if this helps though this can be an uncomfortable procedure that lasts 4-5days.
7. Oral medications: If all of this fails, I would consider trying one of the below drugs. These have higher risks and side effects than above options in general. They are not FDA approved to use in Dry Eye so are being prescribed “off label.”
Some patients may respond to drugs, such as:
a. Naltrexone,
b. Neurontin (gabapentin, Pfizer),
c. Lyrica (pregabalin, Pfizer)
d. Cymbalta (duloxetine, Eli Lilly)
The key side effects I have heard from patients on these drugs is the disturbance of sleep, nightmares, and suicidal ideation. It is important if you are on these medications for dry eye, you tell your family and keep an open dialog with your loved ones and your prescriber if you have any of these side effects.
Safer treatments to try for Neuropathic Dry Eye, which have shown positive improvements are:
1. Autologous Serum
2. Platelet rich plasma.
But most of the patients I have seen on the oral drugs have tried these and they have not work.
We await the results to see if Autologous Stem Cell injections (with or without a combination of PRP) works better than any of the options above.
For now, it is helpful to know you have a component of neuropathic pain and know you are not crazy. It is important to be treated for any associated or underlying anxiety or depression from the pain and have a pain specialist follow you.
A recent patient told me the only place he finds relief from his pain is in a very hot (dry not wet) sauna. Nothing else helps. He has tried some of the oral meds above and they did not help. Only the hot sauna helped.
Why? I do not know, but there must be a way to replicate that pain relief without having to live in a hot sauna.
SLC
References:
1.
The Relationship Between Ocular Itch, Ocular Pain, and Dry Eye Symptoms (An American Ophthalmological Society Thesis).
Abstract
PURPOSE:
METHODS:
RESULTS:
CONCLUSIONS:
- PMID:
- 29391860
- PMCID:
- PMC5774848
Some information on Lyrica
- Confused
- Decreased Blood Platelets
- Infection
- Inflammation Of The Lining Of The Stomach And Intestines
- Puffy Face From Water Retention
- Sensation Of Spinning Or Whirling
- Constipation
- Extreme Sense Of Well Being
- Feeling Weak
- Head Pain
- Injury
- Sinus Irritation And Congestion
- Stomach Cramps
- Twitching
RARE side effects
- Chest Pain
- Difficulty Speaking
- Double Vision
- Dyskinesia
- Giant Hives
- Having Thoughts Of Suicide
- Hemorrhage Of Blood Under The Skin
- Hives
- Low Blood Sugar
- Middle Ear Infection
- Muscle Spasm
- Pink Eye
- Problem Behavior
- Problems With Bladder Control
- Prolonged P-R Interval Observed On EKG
- Rash
- Ringing In The Ears
- Small Skin Blister
- Trouble Breathing
- Visible Water Retention
- Wheezing
- Abnormal Increase In Muscle Tone
- Abnormal Manner Of Walking
- Altered Interest In Having Sexual Intercourse
- Backache
- Bronchitis
- Diarrhea
- Enlarged Breasts
- Feel Like Throwing Up
- Feeling Anxious
- Fever
- Fingernail And/Or Toenail Disease
- Flu-Like Symptoms
- Frequent Urination
- Gas
- Inability To Have An Erection
- Increased Hunger
- Involuntary Eye Movement
- Involuntary Quivering
- Itching
- Joint Pain
- Leg Cramps
- Loss Of Memory
- Loss Of One’s Own Sense Of Reality Or Identity
- Low Energy
- Muscle Pain
- Muscle Weakness
- Nervous
- Numbness
- Problems With Eyesight
- Stupor
- Swelling Of The Abdomen
- Throwing Up
—-
7.
There is no proof published that I can find to date proving gabapentin as a favorable treatment in neuropathic dry eye pain. Still I have many patients that say it works.
Below is the only paper published on Pubmed when I query, “gabapentin neuropathic eye pain.”
———–
8.
When I query: “gabapentin dry eye,” only this comes up.
J Neurol Neurosurg Psychiatry. 2010 Jul;81(7):731-3. doi: 10.1136/jnnp.2009.177303.
Non-length-dependent small fibre neuropathy. Confocal microscopy study of the corneal innervation.
Abstract
BACKGROUND:
OBJECTIVE:
METHODS:
RESULTS:
CONCLUSION:
9.
The same is true when I look for any papers on “pregabalin neuropathic eye pain.” Only these papers have been published.
10.
Topical Naltrexone helps with Corneal Neuropathy?
It may.
Naltrexone is an opiate receptor antagonist and is long lasting. Low Dose Naltrexone (LDN) (4.5 mg daily) has been shown to block opioid receptors temporarily, which in turn leads to improved mood by enhancing endorphin and dopamine activity. It appears to increase β-endorphin, which is an opioid peptide with is known to affect pain modulation and mood via the hypothalamus, and on endocrine secretion.[1]
Topical Application of Naltrexone to the Ocular Surface of Healthy Volunteers: A Tolerability Study.
Abstract
PURPOSE:
METHODS:
RESULTS:
CONCLUSIONS:
Topical Naltrexone as Treatment for Type 2 Diabetic Cutaneous Wounds.
Abstract
No Added Benefit of Duloxetine-Pregabalin Combo in DPNP