When a patient has glaucoma, we have to give drops to regulate and often lower eye pressures in order to save the eye(s)’ vision. These drops though, we have known for years, makes dry eye symptoms worse. More and more studies are showing how glaucoma drops can potentially destroy meibomian glands.
If anyone develops a glaucoma drop that maybe has extra Omega 3 or is shown to save glands, that will be better for patients.
Sandra Lora Cremers, MD, FACS
Cornea. 2017 Dec 8. doi: 10.1097/ICO.0000000000001489. [Epub ahead of print]
Eyelid Changes Related to Meibomian Gland Dysfunction in Early Middle-Aged Patients Using Topical Glaucoma Medications.
Abstract
PURPOSE:
METHODS:
RESULTS:
CONCLUSIONS:
Effects of long-term topical anti-glaucoma medications on meibomian glands
Cornea
First Online: 18 February 2012
- 417Downloads
- Citations
Abstract
Objective
To examine effects of long-term topical anti-glaucoma medications on meibomian gland morphology and function and assess their relationship with slit-lamp findings.
Methods
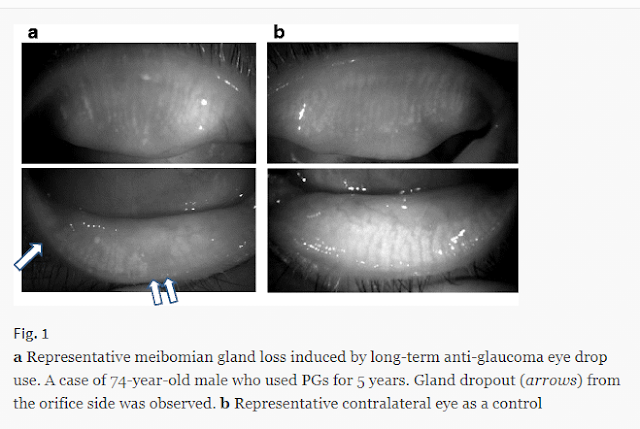
This was a cross-sectional observational case series of 31 patients with glaucoma (mean age ± standard deviation, 65.0 ± 13.0 years; mean duration of eye drop use, 7.9 ± 6.0 years) treated with topical anti-glaucoma drugs in only one eye for more than 1 year: 13 receiving prostaglandin analogues (PGs) alone, eight receiving β-blockers alone, and ten receiving multiple treatments. Untreated contralateral eyes served as controls. Lid margin (lid margin abnormality score: 0–4) and superficial punctate keratopathy (SPK score: 0–1) were observed with a slit lamp. Upper and lower eyelids were turned over to observe meibomian glands using non-contact meibography. Meibomian gland loss was scored for each eyelid from grade 0 (no loss of meibomian glands) through grade 3 (loss >2/3 of total meibomian gland area). Meibomian lipid content (meibum) was scored (meibum score: 0–3).
Results
Treated eyes had significantly higher scores for lid margin abnormality (P = 0.001), SPK (P < 0.001), meibo-score (P < 0.001), and meibum (P < 0.001) than control eyes. Tear film break-up time (BUT) was significantly shorter in treated eyes than in control eyes (P = 0.001). Schirmer values were significantly lower in treated eyes than in control eyes (P = 0.0039). Subgroup analysis indicated a significantly higher meibo-score in eyes treated with PGs (P = 0.0046) and in eyes treated with β-blockers (P = 0.0231) than in the corresponding controls.
Conclusions
Long-term anti-glaucoma eye drop use affects meibomian gland morphology and function.