Sjögren Syndrome
Dry eyes are most commonly NOT due to a significant underlying inflammatory condition. But in patients who also note dryness of the mouth and arthritis with their dry eyes may have a significant underlying inflammatory condition. Dry mouth is informally diagnosed clinically with a question, such as, “are you able to eat saltine crackers [informally noted to be about 7-10] without grabbing a drink of water.” If a patient notes a significant dry mouth on such an occasion, the patient should be evaluated for dry mouth.
It is very important to diagnose Sjogren Syndrome in patients for the following reasons:
1. It gives patients a prognosis regarding their dry eye.
2. It helps MDs understand the need to treat symptoms aggressively compared to a typical dry eye patient.
3. Follow up schedules are more frequent in Sjogren Syndrome patients compared to typical dry eye.
3. Sjogren Syndrome can be associated with other immunological conditions noted below; so it helps to make a patient’s primary MD aware of this.
The key tests to diagnose Sjogrens syndrome are:
1. Antinuclear Antibodies (ANA), which are present in nearly all patients.
2. SS-A and SS-B antibodies (Sjögren’s syndrome A and B antibodies; also referred to as Ro and La antibodies, respectively) found in most, but not all patients,
3. Rheumatoid Factor
4. Thyroid antibodies: Sjögren syndrome patients have an increased frequency of autoimmune thyroid disease with hypothyroidism (10-15%). Lymphocytic infiltration can be observed in the thyroid gland.
5. CBC: a low red blood count (anemia) and abnormal blood levels are markers of inflammation A mild, normochromic, normocytic anemia is present in 50% of patients. Leukopenia occurs in up to 42% of patients.
6. ESR: Erythrocyte sedimentation rate
7. CRP: C-reactive protein
Other blood tests can be helpful if there is clinical suspicion: 20% of Sjogren syndrome patients have other autoantibodies typical of other systemic autoimmune diseases.
8. Anti–Alpha-Fodrin Antibody if suspect juvenile Sjögren syndrome
9. Lupus anticoagulant test (may be present in patients with Primary Sjogren Syndrome and arterial and/or venous thrombosis has been reported in these patients).
10. Anticardiolipin antibodies
11. Anti ̶ salivary duct antibodies are present in most cases of secondary Sjögren syndrome.
12. Type II cryoglobulins are noted, particularly in patients with palpable and nonpalpable vasculitic purpura. Hepatitis C should be sought in these patients.
13. Antibodies to carbonic anhydrase 11 (can be seen in patients with Sjögren syndrome who have primary billiary cirrhosis.)
14. Look for a Negative Serum IgG4 in Sjogren syndrome patients; if positive, think IgG4-related plasmacytic disease (which can mimic the glandular infiltrations of Sjögren syndrome).
———————————–
More information is noted below from MEDSCAPE
Some laboratory tests can be used to assess salivary and lacrimal involvement in Sjögren syndrome. However, no single test is sufficiently sensitive or specific in the diagnosis of Sjögren syndrome. The condition is properly diagnosed only when the results of various tests are simultaneously positive and when subjective symptoms and serologic abnormalities are present.[59]
Laboratory test results may indicate the following:
- Elevated erythrocyte sedimentation rate (ESR)
- Anemia
- Leukopenia
- Eosinophilia
- Hypergammaglobulinemia
- Presence of antinuclear antibodies, especially anti-Ro and anti-La
- Presence of RF
- Presence of anti–alpha-fodrin antibody (reliable diagnostic marker of juvenile Sjögren syndrome)
- Creatinine clearance may be diminished in up to 50% of patients
Multiple autoantibodies are associated with Sjögren syndrome.[60] In a study in which atypical autoantibodies were evaluated in 82 patients with primary Sjögren syndrome, an immunologic overlap (defined by the presence of autoantibodies typical of other systemic autoimmune diseases) was evident in 20% of the patients. The clinical significance of these atypical autoantibodies varied widely.[61]
Patients with primary Sjögren syndrome may have positive test results for lupus anticoagulant and/or anticardiolipin antibodies, and some patients develop clinical events (ie, fetal wastage, arterial and/or venous thrombosis) associated with antiphospholipid syndrome. Anti ̶ salivary duct antibodies are present in most cases of secondary Sjögren syndrome.
Type II cryoglobulins are noted, particularly in patients with palpable and nonpalpable vasculitic purpura. Hepatitis C should be sought in these patients.
In some studies, patients with Sjögren syndrome have an increased frequency of autoimmune thyroid disease with hypothyroidism (10-15%). Lymphocytic infiltration can be observed in the thyroid gland.
Elevations of serum immunoglobulin G4 (IgG4), found in IgG4-related plasmacytic disease (which can mimic the glandular infiltrations of Sjögren syndrome), are not seen in Sjögren syndrome.[62, 63]
Antibodies to carbonic anhydrase 11 can be seen in patients with Sjögren syndrome who have primary billiary cirrhosis.[46]
Schirmer test
The Schirmer test is probably the only test available in the emergency department (ED) that can be used to strongly support or refute suspicion of Sjögren syndrome. A test strip of number 41 Whatman filter paper is placed near the lower conjunctival sac to measure tear formation. Healthy persons wet 15mm or more after 5 minutes. A positive test occurs when less than 5mm are wet after 5 minutes. A Schirmer test is shown in the image below.
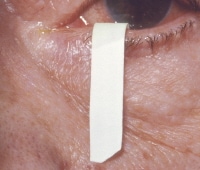 Photograph that demonstrates the Schirmer test, which is used to detect deficient tear production in patients with Sjögren syndrome. The filter paper strip is placed at the junction of the eyelid margins. After 5 minutes, 15 mm of paper should be moistened if tear production is normal, as shown here. Persons older than 40 years may moisten between 10 mm and 15 mm. Patients with Sjögren syndrome have less moistening. Sjögren syndrome is most common in patients with rheumatoid arthritis but may also occur without associated disease and in systemic lupus erythematosus, polyarteritis, systemic sclerosis, lymphoma, and sarcoidosis.
Photograph that demonstrates the Schirmer test, which is used to detect deficient tear production in patients with Sjögren syndrome. The filter paper strip is placed at the junction of the eyelid margins. After 5 minutes, 15 mm of paper should be moistened if tear production is normal, as shown here. Persons older than 40 years may moisten between 10 mm and 15 mm. Patients with Sjögren syndrome have less moistening. Sjögren syndrome is most common in patients with rheumatoid arthritis but may also occur without associated disease and in systemic lupus erythematosus, polyarteritis, systemic sclerosis, lymphoma, and sarcoidosis.
Rheumatoid factor
Rheumatoid factor is present in 52% of patients with primary Sjögren syndrome and in 98% of patients with the secondary disease, occurring even when RA is not present. Consider a diagnosis of RA if the patient has symmetrical polyarticular synovitis. Loss of a previously positive RF finding can be observed in some patients with Sjögren syndrome who develop lymphoma.
Antinuclear antibodies
ANAs are typically present in patients with Sjögren syndrome. Consider the diagnosis of SLE only if symptoms and signs typical of this disorder are present.
Serum protein electrophoresis
Patients with Sjögren syndrome often have a polyclonal gammopathy. Loss of a previously detected polyclonal gammopathy can be observed in some patients with Sjögren syndrome who develop lymphoma. Development of a monoclonal gammopathy can also signal the development of a lymphoma.
Staining
Rose bengal is an aniline dye that stains epithelial surfaces with diminished mucin protection or with exposed epithelial cell membranes. Conjunctival staining can be detected with the naked eye. Slit-lamp examination is performed after rose bengal staining to detect abnormal uptake in the cornea.
Lissamine green staining works similarly but is less irritating to the eye. Fluorescein staining can be used to detect corneal damage.
Salivary testing
Sialometry is a good measure of the degree of decreased salivary flow and helps to establish xerostomia, but the findings do not narrow the differential diagnoses.
Saliva from patients with Sjögren syndrome has elevated levels of sodium, chloride, lactoferrin, and IgA, but these findings are not specific.
Sedimentation rate
The erythrocyte sedimentation rate (ESR) is elevated in 80% of patients with Sjögren syndrome, but the finding is nonspecific.
Protein profiling
Protein profiling (tear proteomics) has revealed reproducible patterns in patients with primary Sjögren syndrome and appears to hold promise as a diagnostic test for this disorder.[64]
Additional test considerations
Other test results to consider are as follows:
- High total protein level or a low albumin level – Should prompt the clinician to perform serum protein electrophoresis
- High alkaline phosphatase level – Should prompt consideration of primary biliary cirrhosis
- Elevated transaminase levels – Consider the possibility of chronic active hepatitis, which can be associated with sicca symptoms, or hepatitis C, which can cause mild salivary gland enlargement; however, mild (< 2-fold) increases in transaminase levels have been observed in 22% of patients with Sjögren syndrome[65]
- Low bicarbonate level – Consider evaluating patients with a low bicarbonate level for type I (distal) renal tubular acidosis; less commonly, patients can also develop proximal renal tubular acidosis with Fanconi syndrome
-
Hypokalemia – This condition, which is occasionally severe enough to lead to periodic paralysis, can be observed in patients with type I renal tubular acidosis; however, it can also be observed in patients who have Sjögren syndrome without renal tubular acidosis[43]Antibodies against SSA/Ro are found in approximately 50% of patients with the disease (75% of patients with primary Sjögren syndrome and 15% of patients with secondary Sjögren syndrome). Thus, the absence of anti-SSA/Ro antibodies does not eliminate the diagnosis of primary or secondary Sjögren syndrome.
Antibodies against SSA/Ro are present in 50% of patients with SLE and are sometimes found in healthy individuals. Thus, the presence of antibody against SSA/Ro cannot by itself be used to establish a diagnosis of Sjögren syndrome.Antibodies against SSB/La are present in 40-50% of patients with primary Sjögren syndrome and in 15% of patients with SLE. Finding antibodies against SSB/La in patients without antibodies against SSA/Ro is unusual, but this combination has occurred in patients with primary biliary cirrhosis and autoimmune hepatitis.Titers of anti-SSA/Ro and anti-SSB/La antibodies do not reflect disease activity. Current enzyme-linked immunosorbent assay tests for these antibodies are more sensitive than previous tests. Thus, the specificity is lower.Antibodies against SSA/Ro are also associated with the annular erythematous lesions of subacute cutaneous lupus. They are also found in the mothers of newborns with neonatal lupus syndromes and congenital heart block, and some of these mothers have or will develop Sjögren syndrome.In patients with Sjögren syndrome, the complete blood count (CBC) is most often within the reference range, but anemia of chronic disease may be present. Pernicious anemia may be associated with the atrophic gastritis.An abnormal white blood cell (WBC) count, especially with an abnormal differential count, should prompt concerns for a lymphoreticular malignancy. In addition, although a low platelet or WBC count can occur in persons with primary Sjögren syndrome, the finding should also prompt consideration for coexisting SLE.A mild, normochromic, normocytic anemia is present in 50% of patients. Leukopenia occurs in up to 42% of patients.In sialography, radiopaque material is injected into the salivary glands. Sialography is useful to exclude the presence of obstructions or strictures, but the diffuse sialectasis of Sjögren syndrome is seen in various other diseases and is therefore not specific.Oil-based contrast medium may not be adequately cleared in patients with Sjögren syndrome and, consequently, may damage adjacent tissues and lead to a chronic granulomatous reaction. Performing this procedure with oil-based contrast should be avoided, especially during episodes of acute swelling.With salivary scintigraphy, the uptake and secretion of sodium pertechnetate technetium-99m (99m Tc) is a gauge of the salivary flow rates and can provide an objective measurement of salivary gland dysfunction. However, the finding of low flow rates is not specific to Sjögren syndrome.Positive findings on either sialography or scintigraphy fulfill a criterion for objective evidence of Sjögren syndrome by the American-European Consensus Group.[2]Minor salivary gland biopsy[66] currently is the best single test to establish a diagnosis of Sjögren syndrome. In this procedure, an incision is made on the inner lip, and some minor salivary glands are removed for examination. In patients with a possible diagnosis of this disease but with severe extraglandular symptoms, a lip biopsy is often performed to firmly establish the diagnosis of Sjögren syndrome. Obtaining the biopsy sample from below normal-appearing mucosa is important in order to avoid false-positive results. At least 4 salivary gland lobules should be obtained for analysis.While this is the most definitive test, performing it is not absolutely necessary from a clinical standpoint. Patients with Sjögren syndrome are essentially treated symptomatically and are observed for the development of other rheumatic disorders or lymphoma. This can be initiated without performing a biopsy. If, however, the diagnosis is in doubt or if a definitive diagnosis is needed, then this is the best test.Salivary gland biopsy can also help to detect pseudolymphoma or lymphoma, as well as the noncaseating granulomas of sarcoidosis.One study showed that not all patients undergoing lip biopsy derived diagnostic benefit from this procedure and that clinical symptoms and serology did not predict a positive lip biopsy.[67]In another study, however, a significant correlation was found between positive findings in minor salivary gland biopsy and the Schirmer test, the rose bengal test, xerostomia, and parotid swelling. The investigators utilized biopsy specimens from the lower lip of 360 patients.[68]Although pathologists use different classification systems, the characteristic findings of minor salivary gland biopsy in a person with Sjögren syndrome include the following (see the image below)[69] :- The biopsy shows focal aggregates of at least 50 lymphocytes, and, to a lesser extent, plasma cells and macrophages
- More than 1 focal aggregate is seen per 4 mm2
- T cells, predominantly CD4+ cells, are present, unlike the predominance of CD8+ T cells seen in the salivary gland biopsy samples from patients with DILS associated with HIV disease
- Normal acini are replaced by lymphocytes
- Focal aggregates are seen in almost all glands
- Ten percent of the lymphocytes are CD5+ B cells that produce IgM and IgG antibodies, often with a monoclonal or oligoclonal pattern
- Large foci are present, possibly showing germinal centers
- Epimyoepithelial islands are uncommon in the minor salivary gland but can be seen in the major salivary glands
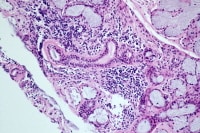 Photomicrograph of a lip biopsy specimen showing two lymphocytic foci adjacent to normal-appearing mucinous acini typical of minor salivary gland abnormalities in Sjögren syndrome.
Photomicrograph of a lip biopsy specimen showing two lymphocytic foci adjacent to normal-appearing mucinous acini typical of minor salivary gland abnormalities in Sjögren syndrome.
A score of greater than 1 focus per 4 mm2 has a specificity of 83.5-95% and a sensitivity of 63-81.8% in the diagnosis of Sjögren syndrome. The focus score may be associated with keratoconjunctivitis sicca, the presence of autoantibodies, and, less commonly, xerostomia.Lymphocytic infiltrates are also seen in other organs. Findings from a gastric mucosal biopsy may show lymphocytic infiltrates with atrophic gastritis. A kidney biopsy may show interstitial lymphocytic infiltration. Lung biopsy can reveal infiltrating CD4+ T cells of a lymphocytic interstitial pneumonitis. Salivary gland biopsy can help to detect pseudolymphoma or lymphoma, as well as the noncaseating granulomas of sarcoidosis.Occlusion of the lacrimal puncta can be corrected surgically. Electrocautery and other techniques can be used for permanent punctal occlusion.During surgery, the anesthesiologist should administer as little anticholinergic medication as possible and use humidified oxygen to help avoid inspissation of pulmonary secretions. Good postoperative respiratory therapy should also be provided. Patients are at higher risk for corneal abrasions, so ocular lubricants should be considered.Biopsies that may be performed in association with Sjögren syndrome include the following:- Minor salivary gland biopsy – For diagnostic purposes
- Parotid gland biopsy – If malignancy is suggested
-
Biopsy on an enlarged lymph node – To help rule out pseudolymphoma or lymphomaSjögren syndrome and its associated disorders necessitate a total patient perspective that is often best provided by an internist. A rheumatologist with specific training and experience in Sjögren syndrome and its associated disorders is also essential to the management of the condition. In addition, good oral prophylaxis and therapy are necessary.Involve ophthalmologists early in the care of patients, for rose bengal and fluorescein staining to help to establish the diagnosis and for assessment of the degree of eye damage.Consultation with an otolaryngologist may be needed early to perform a minor or major salivary gland biopsy if this is deemed necessary to establish a diagnosis. The specialist may also need to perform a parotid biopsy if malignant transformation is suggested.Depending on the problems, patients with Sjögren syndrome may need to be seen by other specialists, including the following:
- Nephrologist – To help manage renal tubular acidosis
- Pulmonologist – To help manage interstitial lung disease
-
Hematologist/oncologist – If pseudolymphoma or lymphoma develops
Approach Considerations
No curative agents for Sjögren syndrome exist. The treatment of the disorder is essentially symptomatic. In secondary Sjögren syndrome, treatment is based on the accompanying disease and its clinical features. Sjögren syndrome and associated SLE improve more than primary Sjögren syndrome. In Sjögren syndrome associated with polymyositis, monthly cyclophosphamide pulse therapy has been used successfully.In annular erythema associated with Sjögren syndrome in Japanese patients, prednisolone (10-20 mg/d) is effective. No evidence-based strategies are available for the management of anular erythema in Western populations because it is rare. However, case reports have demonstrated that hydroxycloroquine can be effective in whites.[70]The inhibition of protease activity in EBV-mediated apoptotic cells may be a potential therapeutic approach in the treatment of Sjögren syndrome.Skin and vaginal dryness
Patients should use skin creams, such as Eucerin, or skin lotions, such as Lubriderm, to help with dry skin. Vaginal lubricants, such as Replens, can be used for vaginal dryness. Vaginal estrogen creams can be considered in postmenopausal women. Watch for and treat vaginal yeast infections.Arthralgias and arthritis
Acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) can be taken for arthralgias. Consider hydroxychloroquine if NSAIDs are not sufficient for the synovitis occasionally associated with primary Sjögren syndrome. However, hydroxychloroquine does not relieve sicca symptoms. Patients with RA associated with Sjögren syndrome likely require other disease-modifying agents.Additional treatment considerations
In patients with major organ involvement, such as lymphocytic interstitial lung disease, consider therapy with steroids and immunosuppressive agents, such as cyclophosphamide.While cyclophosphamide and similar agents may be helpful for treating serious manifestations of Sjögren syndrome or disorders associated with Sjögren syndrome, clinicians should understand that these agents are also associated with the development of lymphomas.Long-term anticoagulation may be needed in patients with vascular thrombosis related to antiphospholipid antibody syndrome.In a small group of patients with primary Sjögren syndrome, mycophenolate sodium reduced subjective, but not objective, ocular dryness and significantly reduced hypergammaglobulinemia and RF.[71]Among the biologic therapies, the greatest experience in primary Sjögren syndrome is with rituximab, an anti-CD20 (which is expressed on B-cell precursors) monoclonal antibody. Anti-B–cell strategies, particularly rituximab, have a promising effect in the treatment of patients with severe extraglandular manifestations of Sjögren syndrome.In a double-blind, randomized, placebo-controlled trial, Meijer et al (2010) found that rituximab significantly improved salivary flow rate, lacrimal gland function, and other variables in patients with primary Sjögren syndrome.[72] In an recent open-label clinical trial, modest improvements were noted in patient-reported symptoms of fatigue and oral dryness, with no significant improvement in the objective measures of lacrimal and salivary gland function despite effective depletion of blood B cells.[73]Rituximab appears promising in the treatment of vasculitis and intravenous immunoglobulin (IVIG)–dependent ataxic neuropathy.[74, 75] Results from the AIR registry (French) indicated that rituximab appears to be effective in cryoglobulinemia or vasculitis-related peripheral nervous system involvement in primary Sjögren syndrome.[76]In a prospective study of 78 patients with primary Sjögren syndrome treated with rituximab, significant improvement in extraglandular manifestations was reported, as measured by EULAR [European League Against Rheumatism] Sjögren Syndrome Disease Activity Index (ESSDAI) (disease activity score) and overall good tolerance reported.[77] Several smaller studies of rituximab revealed improvement of arthralgias, regression of parotid gland swelling,[78] and improvement of immune-related thrombocytopenia.[79]Of the TNF inhibitors, both etanercept and infliximab have failed to demonstrate significant benefit in Sjögren syndrome.Less data are available with regard to the role of anti-CD22, anti-BAFF, anti-IL-1, type 1 interferon, and anti-T–cell agents in treatment of primary Sjögren syndrome, with further investigations ongoing. The overall paucity of evidence in therapeutic studies in primary Sjögren syndromesuggests that much larger trials of the most promising therapies are necessary.Emergency department care
The diagnosis of Sjögren syndrome can be made from the ED if the index of suspicion is high. Patients may present with mild symptoms (eg, eye grittiness, eye dryness or discomfort, dry mouth, recurrent caries). Bilateral parotid gland swelling is also a common presentation.Patients with known Sjögren syndrome should not be taken lightly for their complaint of dry eyes or dry mouth, as these chronic problems can be very distressing and obtrusive.Inpatient care
Give attention to artificial lubricants and humidified oxygen for intubated and/or sedated patients with Sjögren syndrome.Outpatient care
Encourage patients with Sjögren syndrome to be active. In addition, patients should be encouraged to avoid exacerbation of dryness symptoms (eg, through smoking or exposure to low-humidity environments). All patients with Sjögren syndrome should be monitored by an ophthalmologist and dentist, in addition to their rheumatologist. Certain patients may be candidates for punctal occlusion, which is usually performed by an ophthalmologist.Monitoring
Most patients with Sjögren syndrome can be monitored at follow-up visits every 3 months and, if the patient is stable, up to every 6 months. Patients with active problems or in whom an emerging associated illness is a concern can be seen as often as monthly.Dry Eyes
The treatment of dry eyes depends on the severity of the dryness, which is best determined by an ophthalmologist and is graded according to the degree of symptoms, conjunctival injection and staining, corneal damage, tear quality, and lid involvement.[80, 81, 82, 83, 84, 85]New therapeutic strategies designed to facilitate AQP5 trafficking to the apical plasma membrane may prove useful in the management of dry eyes in Sjögren syndrome. In addition, data on novel secretagogues and androgen therapies for dry eyes are promising.[74]Level 1 – Mild symptoms, no corneal signs
Artificial tears should be applied liberally. Patients may need to apply artificial tears more often if they enter a low-humidity environment (ie, air conditioning, airplanes). Artificial tears with hydroxymethylcellulose or dextran are more viscous and can last longer before reapplication is needed. Encourage patients to try various preparations to determine what works best for them.If artificial tears burn when they are instilled, the preservative in the artificial tears is likely irritating the eye. If artificial tears are used more often than every 4 hours, patients should use a preservative-free preparation to avoid eye irritation from the preservatives.The use of humidifiers may help. If the patient is living in an area with hard water, he or she should use distilled water. Patients should avoid medications with anticholinergic and antihistamine effects.Level 2 – Moderate or severe symptoms with tear film signs or visual signs, or mild corneal/conjunctival staining
Patients should use unpreserved tears or gels or nighttime ointments. Patients who wake up in the morning with severe matting in the eyes should use a more viscous preparation (eg, Lacri-Lube) at night. While the more viscous preparations can be applied less often, they can make patients’ vision filmy. Therefore, they are best used at night. The more viscous preparations occasionally lead to blepharitis, which can exacerbate sicca symptoms.The following agents may also be indicated:- Topical steroids
- Secretagogues
- Cyclosporine A[86]
- Nutritional supplements
Level 3 – Severe symptoms with marked corneal changes or filamentary keratitis
The following treatments may be indicated:- Tetracyclines
- Autologous serum tears
- Temporary plugging of the lacrimal puncta to increase the amount of tears that remain in the eyes
Level 4 – Extremely severe symptoms with altered lifestyle, or severe corneal staining, erosions, or conjunctival scarring
The following therapies may be indicated:- Systemic anti-inflammatory therapy, including acetylcysteine
- Topical vitamin A
- Electrocautery and other techniques for permanent punctal occlusion
-
Glasses fitted with moisture shields to decrease evaporation
Dry Mouth
Patients with dry mouth can liberally drink sips of water and take bottled water with them on trips. They can also place a glass of water at their bedside for nighttime use, as needed.[87] Sugar-free lemon drops can also be used as needed to stimulate salivary secretion. Artificial saliva can be used as needed, although patient tolerance varies. Preparations include Salivart, Saliment, Saliva Substitute, MouthKote, and Xero-Lube. Patients should avoid medications with anticholinergic and antihistamine effects.The use of humidifiers may help. Distilled water is best in patients living in an area with hard water.Patients should be seen regularly by a dentist, who may advise fluoride treatments. Toothpaste without detergents can reduce mouth irritation in patients with Sjögren syndrome. Brands include Biotene toothpaste, Biotene mouth rinse, Dental Care toothpaste, and Oral Balance gel.Watch for oral candidiasis and angular cheilitis and treat them with topical antifungal agents, such as nystatin troches. Oral fluconazole may occasionally be needed. Patients also need to be sure to disinfect their dentures.Sinusitis and sinus blockade should be treated because these problems may contribute to mouth breathing. Emphasize the use of isotonic sodium chloride solution nasal sprays to avoid antihistamine use.Pilocarpine or cevimeline tablets are options. Some small studies suggest that interferon alfa may be a useful therapy in the future.

