SVF cells contain the cell types:
1. including adipose-derived stem cells (ADSCs)
2. mesenchymal and endothelial progenitor cells
3. leukocyte subtypes
4. lymphatic cells
5. pericytes
6. vascular smooth muscle cells.
The SVF cells are processed in a way to keep a reproducible and consistent composition of heterogeneous cells that are stable. Upon processing and administration, the adipose-derived SVF cells can differentiate into different tissue types, support neovascularization, replace cells and repair injured issue.
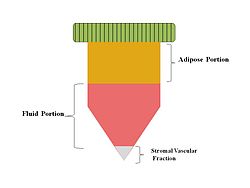
Adipose tissue has emerged as an attractive cell source in tissue engineering and regenerative medicine because it can be easily collected and enriched with stem/progenitor cell populations. The stromal vascular fraction (SVF) derived from adipose tissue contains heterogeneous cell populations such as mesenchymal progenitor/stem cells, preadipocytes, endothelial cells, pericytes, T cells, and M2 macrophages. SVF-derived mesenchymal progenitor/stem cells can be easily expanded in vitro and have the potential to create diverse lineages of cells. Although there have been issues related to their isolation and purification, SVF cells demonstrate regenerative potential in damaged tissues or organs through paracrine and differentiation mechanisms. Furthermore, SVF cells augment immunological tolerance by promoting inhibitory macrophages and T regulatory cells and by decreasing ongoing inflammation. Numerous implantations of freshly isolated, autologous adipose tissue-derived SVF cells in cosmetic surgeries and in a wide variety of other specialties support the safety of SVF cells and have accelerated their clinical application. Despite these attractive advantages of SVF cells in clinical interventions, to our knowledge the recent status of clinical studies of various diseases has not been fully investigated.
Stromal vascular fraction
| Stromal vascular fraction | |
|---|---|
Stromal Vascular Fraction
|
Introduction[edit]
References[edit]
References[edit]
- ^ Riordan, NH; Ichim, TE; Min, WP; Wang, H; Solano, F; Lara, F; Alfaro, M; Rodriguez, JP; Harman, RJ; Patel, AN; Murphy, MP; Lee, RR; Minev, B (Apr 24, 2009). “Non-expanded adipose stromal vascular fraction cell therapy for multiple sclerosis.”.Journal of translational medicine. 7: 29.
- ^ Schipper HS, Prakken B, Kalkhoven E, Boes M. Adipose tissue-resident immune cells: key players in immunometabolism. Trends Endocrinol Metab 2012; 23:407-15.
- ^ Pak, J.; Lee, J. H.; Park, K. S.; Park, M.; Kang, L.-W.; Lee, S. H. (2017). “Current use of autologous adipose tissue-derived stromal vascular fraction cells for orthopedic applications”. J. Biomed. Sci. 24:9
- ^ Pak, J.; Lee, J. H.; Park, K. S.; Jeon, J. H.; Lee, S. H. (2017). “Potential use of mesenchymal stem cells in human meniscal repair: current insights”. Open Access J. Sports Med. 8: 33–38. Open Access J. Sports Med. 8: 33–38.

