The Best Way to Treat Hemorrhoids
Even though I am an eye surgeon, patients and friends ask me about all kinds of medical issues. This is for a dear patient who has been suffering from hemorrhoids for months now and can no longer sleep the pain is so bad.
Hemorrhoids are part of life for many, 50% of the United States population will experience hemorrhoids by age 50. Whether it is the top of the body or the bottom, most MDs will do anything to help their friends and patients find relief of pain.
So here is a summary of the Best Way to Treat Hemorrhoids.
Sandra Lora Cremers, MD, FACS
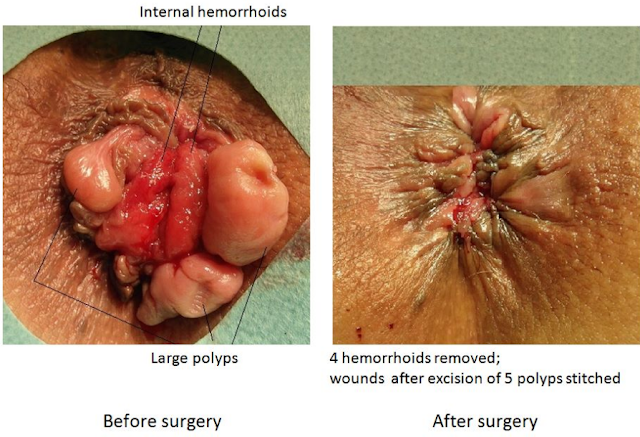
Hemorrhoids are the result of inflamed, swollen veins in your rectum and anus (the hole you poop from). They can be internal (inside) or external (outside the rectum like the photo on the left below.
Hemorrhoids are due to:
1. Straining to have a bowel movement,
2. Constipation,
3. Increases with the elderly
4. Very common in pregnant women.
Though they can be terribly painful, they rarely cause complications.
 The most common symptom for hemorrhoids is the presence of blood &/or feeling a bump on the outside of the rectum. If the hemorrhoid is internal, then the blood will be bright red and will be most noticeable on toilet paper. If external, you could experience a blood clot around your anus or swelling. Overall, common symptoms include:
The most common symptom for hemorrhoids is the presence of blood &/or feeling a bump on the outside of the rectum. If the hemorrhoid is internal, then the blood will be bright red and will be most noticeable on toilet paper. If external, you could experience a blood clot around your anus or swelling. Overall, common symptoms include:- Bleeding
- Swelling
- Itching
- Irritation
- Blood clots or lumps around the anus
- Anal pain
Note that if you incorporate some natural hemorrhoid treatments and follow the prevention tips below, your symptoms may very well disappear as the issue reverses.
Here is the Way the Best Surgeon I know (my cardiothoracic surgeon dad) Would Treat Hemorrhoids:
1. Buy Sitz bath kit: as many you can in warm/hot water. Do at least 4 times per day or everytime you go to the bathroom
A sitz bath is a warm, shallow bath that cleanses the perineum, which is the space between the rectum and the vulva or scrotum. A sitz bath can be used for everyday personal hygiene. It can also provide relief from pain or itching in the genital area.
2. Buy Preparation H and apply according to directions
3. Drink 2 Tablespoons Mineral Oil per day
4. Drink prune juice 1/2-1 cup per day depending on how much it takes to make your stools loose but not too loose.
5. If these do not work, get an Rx for Anusol suppositories (a little capsule you stick up your butt).
6. Take Tylenol for pain as needed. Avoid advil or ibuprofen as will worsen bleeding.
More Natural Remedies Are As Follows:
6 Home Remedies For Hemorrhoids
- Apple Cider Vinegar – Using apple cider vinegar is one of the most popular natural treatments for hemorrhoids. Simply soak a cotton ball or some toilet paper with ACV and apply it to the hemorrhoid area. Repeat this process until the inflammation disappears and symptoms resolve. You should see improvement instantly. Alternatively, add some ACV (half a cup) to a sitz bath.
- Rutin – A health-promoting compound found in numerous plants such as buckwheat, oranges, grapefruit, lemon, cranberries, and asparagus (to name a few), rutin is another home remedy often used for hemorrhoids. Buying it in supplement form may be the best option. One individual on Earthclinic says: “I have had a hemmroid for almost a year now. Just last week I started taking Rutin 500mg twice a day, in the morning and one before going to bed. … taking Rutin for only a week the inflammation has gone down and my hemmroid thankfully is almost gone, it’s less than a size of a pea today.”
- Coconut Oil – Apply coconut oil directly to hemorrhoids, rinse and repeat. In addition to symptoms subsiding, the hemorrhoids should disappear over the course of just a few days.
- Witch Hazel – An astringent and healing tree, witch hazel is one of the oldest known natural remedies for hemorrhoids. Just soak a pad or cotton ball with witch hazel and apply it to the area.
- Aloe Vera – As with the above treatments, simply apply aloe vera to the affected area to relieve symptoms.
- Squat, Don’t Sit – This is actually heavily important and very overlooked. Conventional toilets are highly unnatural, and may be one reason hemorrhoids are rarely seen in less developed countries, where where squatting is done when going to the bathroom. Sitting down to pass a bowel movement puts tremendous strain on the rectum while squatting straightens the rectum and relaxes the puborectalis muscle. This is tip should be done along with any home remedies for hemorrhoids you may use.
Causes And Necessary Prevention Tips – The Best “Treatment”
The most common causes of hemorrhoids are straining during bowel movements and obesity. If you’re straining during bowel movements, there is no doubt that you are suffering from constipation, and obesity only heightens your chance of experiencing these digestive issues. The best solution for hemorrhoids is – you guessed it – to not have them at all!
Follow these essential hemorrhoid prevention tips and you may not even have to delve into any hemorrhoid treatments.
- Exercise and Lose Weight – Being overweight or obese, along with being highly inactive, is the perfect path for a complete decline in health. If you aren’t a healthy weight and aren’t moving, your organs and internal system as a whole becomes sluggish and works at low levels. Start exercising and losing weight to fix the problem and keep your digestive tract working.
- Up Fiber Intake: Eat Plenty of Vegetables, Fruit – Seeing as hemorrhoids result from constipation and straining, it should be no surprise that upping fiber intake can help mend the issue. Fiber helps soften stools and is essential for colon health and digestive health as a whole. This nutrient helps to clean out the gastrointestinal system, preventing constipation and allowing the colon to work at greater levels of efficiency. Sources of fiber include: vegetables of all kinds, flax seeds, almonds, pecans, pistachios, prunes, pears, and beans. Include these foods in your diet while trying the other home remedies for hemorrhoids.
- Take Probiotics and Consume Probiotic-Rich Foods – Probiotics are essential for balancing the bacteria in your gut, which can prevent constipation and absolutely promotes overall health. Either take a high-quality probiotic supplement, or consume more probiotic-rich foods such as fermented foods like fermented cheese, yogurt, sauerkraut, Korean kimchi, and numerous fermented drinks like kombucha tea.
- Hydrate – Staying hydrated with water seems to be the number one recommendation for almost any health ailment. Water helps cleanse your internal system and hydrates your entire body. Along with fiber, drinking more water will help to soften stools and hopefully reduce the need for straining during a bowel movement.
Other Considerations For Hemorrhoid Treatment
- Soaking the area in warm water a few times a day for 10-15 minute periods can reduce inflammation and help relieve symptoms. You may also take a sitz bath and add a half cup of apple cider vinegar.
- Keep the area clean, bathing daily. Don’t use soap on the area as it will likely just cause irritation. Use moist toilet paper to dab the area after a bowel movement to lessen friction from wiping.
- Apply ice packs or cold compresses to relieve swelling.
As always, be sure to share any home remedies for hemorrhoids that work for you, as well as what hasn’t worked for you. It’s important to help natural treatments live on.
Hemorrhoids and what to do about them
Simple treatments to help ease the pain and trouble associated with hemorrhoids or piles.
By midlife, hemorrhoids often become an ongoing complaint. By age 50, about half the population has experienced one or more of the classic symptoms, which include rectal pain, itching, bleeding, and possibly prolapse (hemorrhoids that protrude through the anal canal). Although hemorrhoids are rarely dangerous, they can be a recurrent and painful intrusion. Fortunately, there’s a lot we can do about them.
What are hemorrhoids?
In one sense, everyone has hemorrhoids (or piles), the pillow-like clusters of veins that lie just beneath the mucous membranes lining the lowest part of the rectum and the anus. The condition most of us call hemorrhoids (or piles) develops when those veins become swollen and distended, like varicose veins in the legs. Because the blood vessels involved must continually battle gravity to get blood back up to the heart, some people believe hemorrhoids are part of the price we pay for being upright creatures.
There are two kinds of hemorrhoids: internal ones, which occur in the lower rectum, and external hemorrhoids, which develop under the skin around the anus. External hemorrhoids are the most uncomfortable, because the overlying skin becomes irritated and erodes. If a blood clot forms inside an external hemorrhoid, the pain can be sudden and severe. You might feel or see a lump around the anus. The clot usually dissolves, leaving excess skin (a skin tag), which may itch or become irritated.
Internal hemorrhoids are typically painless, even when they produce bleeding. You might, for example, see bright red blood on the toilet paper or dripping into the toilet bowl. Internal hemorrhoids may also prolapse, or extend beyond the anus, causing several potential problems. When a hemorrhoid protrudes, it can collect small amounts of mucus and microscopic stool particles that may cause an irritation called pruritus ani. Wiping constantly to try to relieve the itching can worsen the problem.
Anatomy of hemorrhoids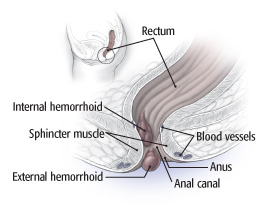
Hemorrhoids are distended blood vessels that form either externally (around the anus) or internally (in the lower rectum).
|
What causes hemorrhoids?
Experts are divided on exactly what causes hemorrhoids, but probably several mechanisms are at work. Traditionally, hemorrhoids are associated with chronic constipation, straining during bowel movements, and prolonged sitting on the toilet — all of which interfere with blood flow to and from the area, causing it to pool and enlarge the vessels. This also explains why hemorrhoids are common during pregnancy, when the enlarging uterus presses on the veins.
More recent studies show that patients with hemorrhoids tend to have a higher resting anal canal tone — that is, the smooth muscle of the anal canal tends to be tighter than average (even when not straining). Constipation adds to these troubles, because straining during a bowel movement increases pressure in the anal canal and pushes the hemorrhoids against the sphincter muscle. Finally, the connective tissues that support and hold hemorrhoids in place can weaken with age, causing hemorrhoids to bulge and prolapse.
_______________________________________________________________________________________________________
Most people take bladder and bowel control for granted — until something goes wrong. An estimated 32 million Americans have incontinence, the unintended loss of urine or feces that is significant enough to make it difficult for them to maintain good hygiene and carry on ordinary social and work lives. The good news is that treatments are becoming more effective and less invasive. This Special Health Report, Better Bladder and Bowel Control, describes the causes… Learn more »
_______________________________________________________________________________________________________
Diagnosing hemorrhoids
Hemorrhoids can usually be diagnosed from a simple medical history and physical exam. External hemorrhoids are generally apparent, especially if a blood clot has formed. Your clinician may perform a digital rectal exam to check for blood in the stool. She or he may also examine the anal canal with an anoscope, a short plastic tube inserted into the rectum with illumination. If there’s evidence of rectal bleeding or microscopic blood in the stool, flexible sigmoidoscopy or colonoscopy may be performed to rule out other causes of bleeding, such as colorectal polyps or cancer, especially in women over age 50.
Home treatment
Most hemorrhoid symptoms improve dramatically with simple, at-home measures. To avoid occasional flare-ups, try the following.
Get more fiber. Add more fiber to your diet from food, a fiber supplement (such as Metamucil, Citrucel, or Fiber Con), or both. Along with adequate fluid, fiber softens stools and makes them easier to pass, reducing pressure on hemorrhoids. High-fiber foods include broccoli, beans, wheat and oat bran, whole-grain foods, and fresh fruit. Fiber supplements help decrease hemorrhoidal bleeding, inflammation, and enlargement. They may also reduce irritation from small bits of stool that are trapped around the blood vessels. Some women find that boosting fiber causes bloating or gas. Start slowly, and gradually increase your intake to 25–30 grams of fiber per day. Also, increase your fluid intake.
Exercise. Moderate aerobic exercise, such as brisk walking 20–30 minutes a day, can help stimulate bowel function.
Take time. When you feel the urge to defecate, go to the bathroom immediately; don’t wait until a more convenient time. Stool can back up, leading to increased pressure and straining. Also, schedule a set time each day, such as after a meal, to sit on the toilet for a few minutes. This can help you establish a regular bowel habit.
Sitz. A sitz bath is a warm water bath for the buttocks and hips (the name comes from the German “sitzen,” meaning “to sit”). It can relieve itching, irritation, and spasms of the sphincter muscle. Pharmacies sell small plastic tubs that fit over a toilet seat, or you can sit in a regular bathtub with a few inches of warm water. Most experts recommend a 20-minute sitz bath after each bowel movement and two or three times a day in addition. Take care to gently pat the anal area dry afterward; do not rub or wipe hard. You can also use a hair dryer to dry the area.
Seek topical relief. Over-the-counter hemorrhoid creams containing a local anesthetic can temporarily soothe pain. Creams and suppositories containing hydrocortisone are also effective, but don’t use them for more than a week at a time, because they can cause the skin to atrophy. Witch hazel wipes (Tucks) are soothing and have no harmful effects. A small ice pack placed against the anal area for a few minutes can also help reduce pain and swelling. Finally, sitting on a cushion rather than a hard surface helps reduce the swelling of existing hemorrhoids and prevents the formation of new ones.
Treat the clot. When an external hemorrhoid forms a blood clot, the pain can be excruciating. If the clot has been present for longer than two days, apply home treatments for the symptoms while waiting for it to go away on its own. If the clot is more recent, the hemorrhoid can be surgically removed or the clot withdrawn from the vein in a minor office procedure performed by a surgeon.
Rubber band ligation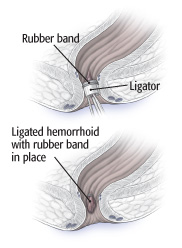
To perform a rubber band ligation, the clinician places a ligator over the hemorrhoid to position a rubber band around its base.
|
Procedures to treat hemorrhoids
Some hemorrhoids can’t be managed with conservative treatments alone, either because symptoms persist or because an internal hemorrhoid has prolapsed. Fortunately, a number of minimally invasive treatments are available that are less painful than traditional hemorrhoid removal (hemorrhoidectomy) and allow a quicker recovery. These procedures are generally performed in a surgeon’s office or as outpatient surgery in a hospital.
Band it. The most commonly used hemorrhoid procedure in the United States is rubber band ligation, in which a small elastic band is placed around the base of a hemorrhoid (see bow above). The band causes the hemorrhoid to shrink and the surrounding tissue to scar as it heals, holding the hemorrhoid in place. It takes two to four procedures, done six to eight weeks apart, to completely eliminate the hemorrhoid. Complications, which are rare, include mild pain or tightness (usually relieved with a sitz bath), bleeding, and infection. Other office procedures include laser or infrared coagulation, sclerotherapy, and cryosurgery. They all work on the same principle as rubber band ligation but are not quite as effective in preventing recurrence. Side effects and recurrence vary with the procedure, so consult your physician about what’s best for your situation.
Hemorrhoidectomy. You may need surgery if you have large protruding hemorrhoids, persistently symptomatic external hemorrhoids, or internal hemorrhoids that return despite rubber band ligation. In a traditional hemorrhoidectomy, a narrow incision is made around both external and internal hemorrhoid tissue and the offending blood vessels are removed. This procedure cures 95% of cases and has a low complication rate — plus a well-deserved reputation for being painful. The procedure requires general anesthesia, but patients can go home the same day. Patients can usually return to work after 7–10 days. Despite the drawbacks, many people are pleased to have a definitive solution to their hemorrhoids.
Staples. An alternative to traditional hemorrhoidectomy is called stapled hemorrhoidopexy. This procedure treats bleeding or prolapsed internal hemorrhoids. The surgeon uses a stapling device to anchor the hemorrhoids in their normal position. Like traditional hemorrhoid removal, stapled hemorrhoidopexy is performed under general anesthesia as day surgery, but it’s less painful and recovery is quicker.

