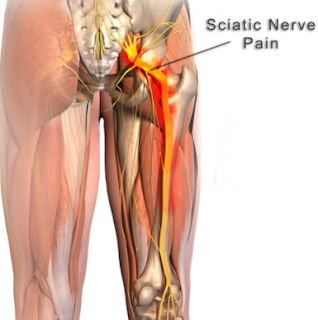
Sciatica Nerve Pain or Sciatica is a common type of pain affecting the sciatic nerve. The Sciatic Nerve is a large nerve extending from the lower back down the back of each leg. Sciatica is caused by direct compression or the nerve or irritation of the root(s) of the lower lumbar and lumbosacral spine.
Top 10 Causes of Sciatic Nerve Pain are:
1. Being overweight: extra tissues & fat put pressure on exit path of the sciatic nerve.
2. Pregnancy
3. Muscle spasm in the back or buttocks
4. Herniated Disc or Degenerative disc disease (breakdown of discs, which act as cushions between the vertebrae)
5. Lumbar spinal stenosis (narrowing of the spinal canal in the lower back)
6. Spondylolisthesis (a condition in which one vertebra slips forward over another one)
7. Muscle spasm in the back or buttocks
8. Trauma or Previous Trauma
9. Tumor: this is rare thank goodness, but tumors can compress the sciatic nerve and cause low back pain.
10. Appendicitis: this is rare, but a smoldering appendicitis can begin as low back pain which can be mistaken for sciatica. Usually appendicitis is rapid/acute and does not radiate down the leg. Very severe pain when you touch inside the belly button may be a sign of an “acute abdomen” (ie, a dangerous process inside the belly).
11. Abdominal aneurysm (a bulge in the aorta which can be life threatening): it is rare for an aneurysm to cause sciatica.
12. Diet related inflammation of nerve: this is likely much more common than some of the above on the list. Still many MDs question the role of diet in nerve related pain. For many patients, it is likely a contributing factor that takes them over the edge into daily pain.
Sciatic Nerve pain can take days-months to heal depending on the cause. In some patients, their diet can make nerve pain worse.
Top 6 Tests You Should Get If You Have Chronic Back Pain:
1. Urinalysis: this makes sure your kidneys are not the cause.
2. Complete blood count (CBC)
3. Erythrocyte sedimentation rate (ESR): A CBC & ESR, especially if you have fevers off and on, makes sure there is no hidden inflammation in the body as a cause. It would be very elevated if you had a dangerous condition, such as an epidural or spinal abscess, or osteomyelitis.
4. Ultrasound: you may need an ultrasound if you have suspected appendicitis, a pathologic (ie, you have a tumor) pelvic process, or abdominal aneurysm (a bulge in the aorta which can be life threatening).
5. CT Scan: you may need a CT based on the criteria below.
6. MRI: you may need an MRI based on the criteria below.
The American College of Radiology (ACR) has recommends the following for chronic low back pain:
-
Uncomplicated acute low back pain and/or radiculopathy are benign, self-limited conditions that do not warrant any imaging studies.
-
MRI of the lumbar spine should be considered for those patients presenting with red flags raising suspicion for a serious underlying condition, such as cauda equine syndrome, malignancy, or infection.
-
In patients with a history of low-velocity trauma, osteoporosis, or chronic steroid use, initial evaluation with radiographs is recommended.
-
In the absence of red flags, first-line treatment for chronic low back pain remains conservative therapy with both pharmacologic and nonpharmacologic (eg, exercise, remaining active) therapy.
-
If there are persistent or progressive symptoms during or following 6 weeks of conservative management and the patient is a surgery or intervention candidate or diagnostic uncertainty remains, MRI of the lumbar spine has become the initial imaging modality of choice in evaluating complicated low back pain.
-
MRI is the imaging procedure of choice in patients suspected of cord compression or spinal cord injury.
-
Patients with recurrent low back pain and history of prior surgical intervention should be evaluated with contrast-enhanced MRI.
Lumbosacral spine series are expensive and expose the reproductive organs to significant radiation. Annually, 7-8 million such tests are obtained, but most have little value in directing therapy, particularly among adults younger than 50 years. Osteophytes are the most frequently seen abnormality of plain films followed by intervertebral disc space narrowing. Both increase with age. Disc space narrowing appears to be more frequent in women. Disc space narrowing at 2 or more levels is strongly associated with back pain pathology.
Unless a history of traumatic injury or systemic illness is present, such films should be obtained only for suspicion of malignancy or infection. Malignant involvement of vertebral bodies can be evident on plain film when as little as 30% of the vertebral body has been replaced. Other indications that suggest the need for radiographic imaging include chronic steroid use and acute onset of pain in patients older than 50 years or in the pediatric age group. The physician may also consider obtaining radiographs in patients whose cases involve (or potentially involve) litigation or for patients seeking compensation.
CT and MRI are generally considered the studies of choice for more precise imaging of the vertebrae, paraspinal soft tissues, discs, or spinal cord. CT images cortical bone with higher resolution and can delineate some fractures better than MRI. MRI is generally the preferred imaging modality for detecting disc, cord, or soft tissue abnormalities. See the image below.
 Magnetic resonance image of the lumbar spine. This image demonstrates a herniated nucleus pulposus at multiple levels.
Magnetic resonance image of the lumbar spine. This image demonstrates a herniated nucleus pulposus at multiple levels.
Ultrasonography may be useful if the differential diagnosis includes appendicitis, a pathologic pelvic process, or abdominal aneurysm.
True emergencies that necessitate imaging include the following:
-
Patients with a history of malignancy and new evidence of nerve entrapment
-
Patients with back pain associated with paralysis or gross muscle weakness
-
Patients with bilateral neurologic deficits associated with bowel or bladder function loss
-
Patients in whom an epidural hematoma or epidural abscess is suspected
-
Postoperative patients with a recent lumbar laminectomy or hip replacement
Improvement occurs in almost all patients within 4-6 weeks, except those with infection, occult malignancy, or systemic illness. If pain fails to significantly improve or resolve in this time frame, imaging is always indicated. Reference: http://emedicine.medscape.com/article/822462-workup#c6
Top Ten Treatments of Sciatic Nerve Pain (Sciatica)
Sciatic nerve pain can last hours to years. It depends on cause and your treatment. Here are the top ways to stop or lessen the pain. If the pain is chronic, keep a Pain Diary to help find the triggers.
1. Loose weight & Eat a low Inflammatory or No Inflammatory Diet:
This can be hard to do, but try a low carb, gluten free diet to shed the pounds. If you are pregnant, the delivery of the baby will help. Still the added pounds can cause the pain to stay, so start loosing the weight with a good anti-inflammatory diet https://drcremers.com/2016/12/anti-inflammatory-diet-best-initial.html AND increase gradually your exercise regimen with the advice of your doctor.
Do not forget that loosing the “water weight” can also help. Avoid salty foods as well.
2. Ice or Heat
Apply an ice pack or a heating pad as needed for 15 minutes. Ice tends to decrease inflammation better, but some patients note that the heating pad helps. Heat likely helps as it relaxes surrounding muscles which in turn decrease exertion on the surrounding tissue. Ice or Heat may not help in some patients who are particularly overweight as the sciatic nerve is buried deep within the buttock and leg. Still, this is cheap and has no risk. And for many it helps relieve the pain without drugs.
3. Exercise and Physical Therapy

Exercise may be the last thing you want to do when you have sciatica, but exercise is key. Physical activity increases blood flow to the disk and the nerve. This helps decrease inflammation which can lead to scar tissue and chronic pain. Take 15- to 20-minute walks. If that hurts too much, give swimming or water aerobics a try. When you are in the water, there is less pressure on your nerves. I
4. See a physical therapist, who can prescribe stretching exercises to restore flexibility to the back or moves that strengthen core muscles, helping to stabilize the spine and reduce the likelihood of a similar injury.
5. Massage:
Massage can help relax the muscle that contracts and adds to the pain. More info at prevention.com: Jeff Smoot, vice president of the American Massage Therapy Association. The sciatic nerve sits underneath a muscle called the piriformis, which is located beneath the glutes. “When the piriformis muscle gets tight, it pinches the sciatic nerve, causing tingling and numbness down into the leg,” says Smoot. He applies pressure to irritated and inflamed areas, or trigger points, in the piriformis muscle, as well as in muscles in the lower back and glutes. Typically, Smoot schedules treatments 7 to 10 days apart. If patients don’t see progress by the fourth visit, “they need to try another form of therapy,” he says. http://www.prevention.com/health/health-concerns/best-treatments-sciatic-nerve-pain
6. Yoga: some Yoga can help. Personally, I prefer to stay away from the spiritual aspect of Yoga in favor of Old Testament and New Testament beliefs and prayers. Still the stretching in Yoga can be beneficial for many things. I would just be saying the Rosary while doing Yoga 😉
 ( Photograph by Peter Augustin/Getty Images )
( Photograph by Peter Augustin/Getty Images )
A study in the journal Pain reported that people with chronic back pain who practiced Iyengar yoga for 16 weeks saw pain reduced by 64% and disability by 77%. Although yoga’s effects on sciatica are less clear, gentle forms may be beneficial. By strengthening muscles and improving flexibility, a yoga practice can help sciatica sufferers “move and function better so they don’t fall into a posture that aggravates the sciatica,” says James W. Carson, PhD, a psychologist at the Comprehensive Pain Center at Oregon Health & Science University. For extra grip and stability, try these grip socks from Natural Fitness.
7.
St. John’s wort oil:
This is a topical treatment or liniment: a liquid or lotion, especially one made with oil, for rubbing on the body to relieve pain. This has not been studied in a randomized, prospective, double blinded trial. At least I could not find a good study. It should do little to no harm, though, if tried. Apply the anti-inflammatory oil two or three times a day where there’s pain. Another option: an OTC cayenne pepper plaster or cream; capsaicin, found in chiles, hinders the release of pain-causing compounds from nerves. For severe cases, Low Dog uses the prescription chile patch Qutenza, designed for shingles pain. “One application is effective for weeks,” says Low Dog.
8. Devil’s Claw
This has also not been studied in a randomized, prospective, double blinded trial. At least I could not find a good study. It should do little to no harm, though, if tried.
 ( Photograph by Dorling Kindersley/Getty Images )
( Photograph by Dorling Kindersley/Getty Images )
The herbal medication devil’s claw is “quite a potent anti-inflammatory, working like ibuprofen and similar drugs to inhibit substances that drive inflammation,” says Low Dog. She generally starts patients on 1,500 to 2,000 mg twice a day. Look for a brand that has a standardized extract of roughly 50 mg of harpagoside, the active compound. Safety reviews show that the supplement is well tolerated by most people but should be avoided by patients with peptic ulcers or on blood-thinning medications.
9. Pain Relievers and Muscle Relaxants
Taking a nonsteroidal anti-inflammatory drug, either OTC (like ibuprofen) or Rx, can ease the distress. Because painful muscle spasms may also accompany a disk herniation, doctors sometimes prescribe muscle relaxants or pain-reducing tricyclic antidepressants. A caveat: “These won’t help with the pain caused by pressure on the sciatic nerve,” says A. Nick Shamie, MD, a spokesperson for the American Academy of Orthopaedic Surgeons.
10. Acupuncture
Acupuncture does work. Pushing on pressure points around a nerve can help as well. If there is no severe damage to your nerve based on an MRI or mild symptoms, putting pressure directly on the area of pain until it hurts a bit sometimes will help relieve the pain permanently. I have done this with sciatic pain when I was pregnant and with mounting headache pain at the pressure points at the superior orbital notch.
From http://www.prevention.com/health/health-concerns/best-treatments-sciatic-nerve-pain: “You can get relief as soon as the first session, though it takes about 12 sessions to see improvement,” says Jingduan Yang, MD, assistant professor at the Jefferson Myrna Brind Center of Integrative Medicine at Thomas Jefferson University. A small study in the Journal of Traditional Chinese Medicine found that of 30 people with sciatica, 17 got complete relief and 10 saw symptoms improve with warming acupuncture, in which the needles are heated.
11. TENS unit therapy
Most of my friends and patients know I am all into natural remedies. For all my pregnancies, I used an electric massager for my back to help with back pain during labor and for post-delivery uterine cramping (which in some cases was worse than the delivery). I avoided all pain meds as I wanted to deliver as naturally as possible. Though I have never used the TENS unit, I know it works for many patients.
TENS unit therapy utilizes a small battery-operated remote attached by wires to pads or electrodes. The electrodes are placed strategically on the body, and the TENS unit transmits an electric current.
For the best results, the electrodes are positioned near the painful area or on a pressure point that reaches to the painful area. For example, for radiating leg pain, the TENS patch might be placed on the low back. The electrical current is controlled by a battery-operated pack the size of a deck of playing cards. The current can be administered continuously or at timed intervals, depending on the recommendation of the therapist or doctor.
TENS unit therapy may be used for patients who are suffering from:
- Sciatica pain
- Osteoarthritis
- Post-operative musculoskeletal pain
- Diabetic neuropathy
- Frozen shoulder syndrome
- Migraines
This treatment has become so popular that patients can now purchase much more affordable over-the-counter TENS units. Even if patients choose to supply their own TENS unit, it is important to work closely with a doctor to monitor this treatment. More information: https://paindoctor.com/tens-unit-therapy-as-sciatica-treatment/
12. Epidural Steroid Injections
People whose pain doesn’t lessen within about a month and who aren’t helped by other therapies may find their pain remedied by an x-ray-guided injection of steroid into the lower back near the sciatic nerve, says Raj Rao, MD, a spokesperson for the AAOS. “The hope is to reduce inflammation within that nerve branch,” explains Rao. Because of concerns about side effects, such as loss of bone density, the epidural shots are limited to three a year. http://www.prevention.com/health/health-concerns/best-treatments-sciatic-nerve-pain
13. Chiropractic Care
For some reason, many doctors I know are a little skeptical of chiropractic care. I have many friends who love their chiropractor. President Kennedy had a Chiropractor. More and more studies are showing that some patients do benefit from chiropractic care. Sixty percent of people with sciatica who didn’t get relief from other therapies and then tried spinal manipulation experienced the same degree of pain relief as patients who eventually had surgery, found a 2010 study in the Journal of Manipulative and Physiological Therapeutics. The 120 people in the study saw a chiropractor about 3 times a week for 4 weeks, and then continued weekly visits, tapering off treatment as they felt better. In people who responded to chiropractic care, benefits lasted up to a year. “Spinal manipulation may create a response in the nervous system that relieves pain and restores normal mobility to the injured area,” says study researcher Gordon McMorland, DC, of National Spine Care in Calgary, Alberta. “It also reduces inflammation, creating an environment that promotes the body’s natural healing mechanisms.” Just be careful to go to a reputable chiropractor just as you would to an MD. http://www.prevention.com/health/health-concerns/best-treatments-sciatic-nerve-pain
14. Surgery
I would recommend you try all of the above before you have surgery. Still there are many who need surgery to have pain relief. After 4 to 6 weeks of unremitting symptoms, patients may qualify for surgery. The Spine Patient Outcomes Research Trial found that those who had surgery for a herniated disk had greater decreases in pain and disability 3 months afterward than patients who did not. The benefits lasted up to 4 years.
15. For those who have tried everything and are still in chronic pain: Get a Pain Clinic Consultation. The MDs there are usually amazing and have many options
 Magnetic resonance image of the lumbar spine. This image demonstrates a herniated nucleus pulposus at multiple levels.
Magnetic resonance image of the lumbar spine. This image demonstrates a herniated nucleus pulposus at multiple levels. ( Photograph by Peter Augustin/Getty Images )
( Photograph by Peter Augustin/Getty Images ) ( Photograph by Dorling Kindersley/Getty Images )
( Photograph by Dorling Kindersley/Getty Images )