It is important to remember a dry tear film or unstable tear film can make these mild dysphotopsias worse. Thus it is important to have the best tear film possible before and after surgery. Treating dry eye and meibomian gland dysfunction is crucial before cataract surgery as a patient with 20/20 vision could still be miserable and feel the quality of vision is poor even though the quantity is perfect.
Dysphotopsias are common complaints in patients who have cataracts. Additionally, previous eye trauma, laser refractive surgery (not uncommon), laser iridotomy for narrow angle (uncommon), blue eyes (not uncommon), and any other eye surgery can cause such symptoms.
a. A whitish shadow around object can result from the type of implant choosen: diffractive multifocal IOL can cause halos.
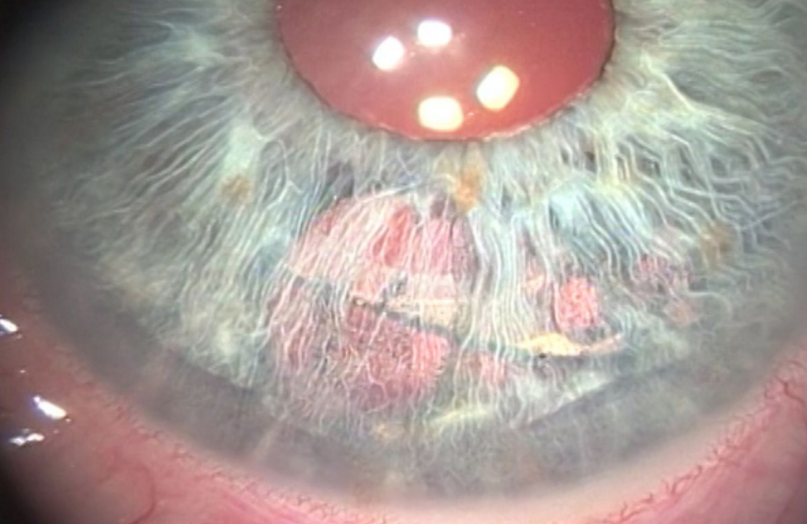
b. Posterior Capsular Opacification (PCO): proliferative lens fibers can cause the halos or streaking; this happens in 30-40% of patients after surgery and is quickly correctable with Yag laser in the office. usually result from small spheres of water in the epithelium and indicate elevated IOP.
c. Blue colored iris: I have seen patients with a Monofocal implant (not a multifocal) not the persistent of halos even after cataract surgery (many patients note halos and glare with dense cataracts), and continued to have them after cataract surgery despite a normal cornea, retina, and opened capsule.
d. More common in patients who have had a hydrophobic lenses: I don’t use these ever.
e. Also can be due to misdirected light rays from internal reflections and the anterior or posterior sharp IOL edge.
2. Glare:
a.Usually due to scattering of light that is diffused as a result of lens fibers or foamy degeneration of lens epithelial cells.
b. Fuch’s Dystrophy: abnormalities or loss of corneal endothelial cells.
c. More common in patients who have had a hydrophobic lenses: I don’t use these ever.
d. Also can be due to misdirected light rays from internal reflections and the anterior or posterior sharp IOL edge.
3. Chromatic halos or Rainbow:
a. Can result from small spheres of water in the corneal epithelium
b. Can indicate elevated intraocular pressure.
c. Microcystic edema and a femtosecond laser spot pattern resulting from use of an older femtosecond laser are can rarely cause such halos.
d. A decentered diffractive multifocal IOL can cause halos
4. Streaks:
a. could be you have astigmatism or high plus cylinder from either
-corneal aberrations: the cornea can change its shape after eye surgery or with aging and eye rubbing.
b. tilted implant: this can be determined if the cornea keratometer or Pentacam shows no astigmatism but the refraction shows significant astigmatism.
c. Posterior Capsular Opacification (PCO): proliferative lens fibers can cause the streaking; this happens in 30-40% of patients after surgery and is quickly correctable with Yag laser in the office.
5. Crescents:
a. could be due to you seeing the implant (intraocular lens or IOL)’s edge. The IOL may be decentered and light is coming through the aphakic (missing implant part) pupil and the IOL.
b. Patients who have had a previous laser iridotomy may notice the edge of an IOL if the iridotomy is very big or the iris was chaffed during cataract surgery.
6. Rings:
a. These often occur if you have had a refractive multifocal IOLs,
a. Can result from scattering of light that is diffused as a result of lens fibers or foamy degeneration of lens epithelial cells.
a. Can be due to glistening formation in the IOL.
1. Depending on the cause, the following are effective treatments if the symptoms do not go away or are severe.
a. Corneal Tattoo: Does not require a repeat intra-ocular surgery and is very safe. May not be effective for some causes.
b. Remove the nasal annulus of the overlying anterior capsule
c. IOL exchange or place the shoulders of the haptics horizontally with the one-piece IOL
d. Exchanging the IOL for a rounded-edge silicone IOL
e. Implant a secondary piggyback IOL in the sulcus
f. Reversing optic capture
g. Iris suture fixation of the capsule bag IOL complex.
h. Sutureless, glued IOL exchange
i. Morcher ring or Aniridia ring segment
Acta Medica Marisiensis 2017;63(1):15-18 DOI: 10.1515/amma-2017-0002
The Prevalence of Dysphotopsia in Patients with
Recent Cataract Surgery
Andreea Dana Fişuş¹*
, Zoltán Madaras¹, Karin Ursula Horváth¹,
²
¹ Tîrgu Mureş County Hospital, Ophthalmology Clinic
² University of Medicine and Pharmacy Tîrgu Mureş
Pseudophakic dysphotopsia are becoming increasingly important as unwanted side effect after cataract surgery. Objective: The purpose of
this study is to compare the photic symptoms experienced by patients after cataract surgery. Material and method: This is a prospective
study that included 105 eyes from 99 patients, which underwent uncomplicated phacoemulsification and IOL implantation, between June
2015 and June 2016, performed at Ophthalmology Clinic Tg Mureș. Patients without visually consequential ocular co-morbidity completed a
questionnaire, designed to assess subjectively perceived visual functioning and identify symptoms of dysphotopsia. Results: From the total
number of patient, hydrophobic lenses were implanted in 95 patients and 10 patients received hydrophilic lenses. Photic effects were reported
in 18% of treated eyes. Although the percentage of dysphotopsia is higher in the hydrophobic lenses category, there was no significant statistical
difference between the two categories. Conclusion: The incidence and significance should not be overlooked, thus visual acuity is not
enough for evaluating postoperative visual function.