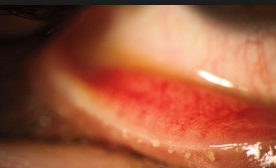
Stem cell use remains controversial in many fields of medicine and surgery. As noted in previous posts, we know that limbal stem cells work for limbal stem cell deficiency and corneal scar tissue/vision loss from chemical burns, Stevens Johnson Syndrome, and Graft Versus Host Disease. I and thousands of surgeons across the world have been performing limbal stem cell transplants for years. This is safe, effective surgery with very few risks. The biggest risk is that the graft rejects and has to be repeated or the limbal stem cell transplant does not help enough to restore vision or provide relief. Most of these patients need multiple treatments to achieve vision improvement and pain relief.
Limbal stem cell transplantation works, but it is considered as one of the last options given the complexity of the surgery and recovery time.
I have spoke to two surgeons in California who have used autologous, adipose derived stem cells for a patient with Stevens Johnson Syndrome with reported good results as the patient was able to return to work after having been out of work for years. Still they have not published this 1 case report yet.
I have also emailed with Dr. Paul Vickers in Australia on his use of autologous, adipose derived stem cells for dry eye and neuropathic pain. He also reports good results but still no randomized, controlled study has been published.
It will take years before a well done, controlled study can be performed. In the meantime, thousands of patients, in efforts to find pain relief, continue to use many medications which have side effects (eg., steroids for dry eye which cause cataracts and glaucoma when used for a period of time–in some it can be weeks, in others it can me months-years).
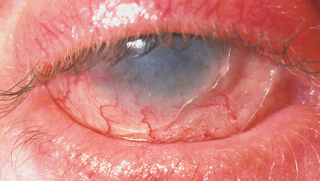
Currently we have 2 patients who had autologous, adipose derived stem cells for dry eyes. Both patients report significant improvement in their symptoms since the procedure. One of them felt as if there was a “red hot line” around her whole body which she said seemed to feel like inflammation as if she would “catch something on fire if she touched it.” This has resolved since the use of the stem cells. Also the eye that was treated feels better compared to the eye that was not treated. This is great news, but we still wait for the post-operative meibography.
Similarly, the other patient reports improvement after the autologous, adipose derived stem cells treatment after about 6 weeks. This patient notes that he had tried Xiidra and Azithromycin drops in the past without relief. Now when he uses them, he has finally relief and is able to even sleep without pain.
These are only 2 cases and still to early to draw a conclusion. Neither patient had any side effects.
Time will tell if this is a long term solution.
Sandra Lora Cremers, MD, FACS