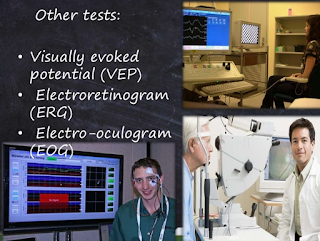
VEP (Visual Evoked Potential) and ERG (Electroretinogram)
A Visual Evoked Potential is an evoked potential caused by a visual stimulus, such as an alternating checkerboard pattern on a computer screen. Responses are recorded from electrodes that are placed on the back of your head and are observed as a reading on an electroencephalogram (EEG). These responses usually originate from the occipital cortex, the area of the brain involved in receiving and interpreting visual signals.
When is the VEP used?
A doctor may recommend that you go for a VEP test when you are experiencing changes in your vision that can be due to problems along the pathways of certain nerves. Some of these symptoms may include:
- Loss of vision (this can be painful or non-painful);
- Double vision;
- Blurred vision;
- Flashing lights;
- Alterations in colour vision; or
- Weakness of the eyes, arms or legs.
These changes are often too subtle or not easily detected on clinical examination in the doctor’s surgery. In general terms, the test is useful for detecting optic nerve problems. This nerve helps transfer signals to allow us to see, so testing the nerve allows the doctor to see how your visual system responds to light. The test is also useful because it can be used to check vision in children and adults who are unable to read eye charts.
What does the VEP detect?
The VEP measures the time that it takes for a visual stimulus to travel from the eye to the occipital cortex. It can give the doctor an idea of whether the nerve pathways are abnormal in any way. For example, in early or established glaucoma, the nerve connection may be affected. In multiple sclerosis, the insulating layer around nerve cells in the brain and spinal cord (known as the myelin sheath) can be affected. In MS, it takes a longer time for electrical signals to be conducted from the eyes, resulting in an abnormal VEP. A normal VEP can be fairly sensitive in excluding a lesion of the optic nerve, along its pathways in the anterior part of the brain.
ERG is a diagnostic test that measures the electrical activity of the retina generated by neural and non-neuronal cells in the retina in response to a light stimulus or a pattern of light stimuli. The electrical response is a result of biochemical process in which a retinal potential generated by light-induced changes in the flux of transretinal ions, primarily sodium and potassium. Most often, ERGs are obtained using electrodes embedded in a corneal contact lens or electrodes placed around the eye, which measure a summation of retinal electrical activity at the corneal surface.
http://www.diopsys.com/patients/erg-testing
Frequently Asked Questions about
Visual Electrophysiology and Eye Diseases
If you don’t see the information you need below, please contact us.
General Information
Eye and Vision Disorders
General Information
What is a Diopsys VEP Vision Test?
It is a painless, safe, non-invasive vision test to objectively measure neurological responses of the entire visual pathway using visual evoked potential (VEP) technology. It is much more than a common vision test.
What is Visual Evoked Potential (VEP)?
Visual Evoked Potential is a non-invasive testing method that provides objective information about the function of the entire vision system. VEP provides a means to measure the complete visual pathway, from the lens to the visual cortex, to detect mechanical or neural abnormalities related to vision. These problems are often subtle and difficult to detect.
The VEP is an electrical signal generated in response to a known visual stimulus. The potential is an electrical response to a stimulus. The Diopsys® VEP Vision Testing Systems use visual stimuli in different patterns and contrasts to evoke the electrical response, or potential, in the brain.
How should I prepare for the test?
All medications should be taken as usual unless otherwise directed by the doctor. Hair should be clean, dry, and free of any gels, sprays, or oils.
It is important that you feel relaxed and comfortable so the test results are accurate. For young children it may be helpful to bring a favorite item such as a blanket, pacifier, or toy that will make them feel more comfortable.
The technician will attach three small sensory pads to your head using a washable gel material. You will be seated in front of a screen and asked to stare at the center. The screen will display different size patterns that quickly reverse. One eye may be covered while the other eye is tested. A computer records your response. The testing time may vary depending on what tests your doctor orders.
What else do I need to know?
You must sit still during the test. Relaxation is an important part of the test.
What can I expect after the test?
After the test the technician will remove the sensory pads and use a small amount of water to remove any gel residue. The test results will be given to your doctor.
Ophthalmologist vs Optometrist
Wondering if your eye care specialist is an optometrist or ophthalmologist? Doctors of optometry (ODs) examine, diagnose, treat, and manage diseases, injuries, and disorders of the visual system, the eye, and associated structures as well as identify related systemic conditions affecting the eye.
An ophthalmologist is a medical doctor (MD) or doctor of osteopathy (DO) specializing in the treatment of diseases of the eye and vision, covering the full spectrum of eye care, from prescribing lenses to complex and delicate eye surgery.
These FAQ’s are not specific to any patient but provides general inform. For questions about your or your relative’s test, please ask the eye care specialist in charge of your vision care.
Eye and Vision Disorders
What is glaucoma? What causes glaucoma?
According to the Glaucoma Research Foundation, glaucoma is a group of eye diseases that gradually steal sight without warning. In the early stages of the disease, there may be no symptoms. Experts estimate that half of the people affected by glaucoma may not know they have it.
Vision loss is caused by damage to the optic nerve. This nerve acts like an electric cable with over a million wires. It is responsible for carrying images from the eye to the brain. There is no cure for glaucoma yet. However, medication or surgery can slow or prevent further vision loss. Early detection is vital to stopping the progress of the disease.
Signs and Symptoms of Glaucoma
Depending on the type of glaucoma you have, you may experience a gradual loss of peripheral vision, tunnel vision, halos around lights, blurred vision, severe eye pain, sudden onset of visual disturbance, often in low light, and reddening of the eye.
Do not wait to visit your eye doctor until you have a problem because in the early stages of the disease, there may be no symptoms. Regular eye exams are the key to detecting glaucoma early enough for successful preventive treatment.
What is diabetic retinopathy?
The National Eye Institute defines diabetic retinopathy as an eye disease that causes changes in the blood vessels of the retina that results as a complication of diabetes. In some people with diabetic retinopathy, blood vessels may swell and leak fluid. In other people, abnormal new blood vessels grow on the surface of the retina.
In the early stages of the disease, there may be no symptoms; but, over time, diabetic retinopathy can get worse and cause vision loss. Diabetic retinopathy usually affects both eyes.
Signs and Symptoms of Diabetic Retinopathy
Blurred vision may occur when the macula—the part of the retina that provides sharp central vision—swells from leaking fluid. This condition is called macular edema. If new blood vessels grow on the surface of the retina, they can bleed into the eye and block vision. You may see a few specks of blood, or spots, “floating” in your vision.
Do not wait to visit your eye doctor until you have a problem because there are often no symptoms in the early stages of the disease. Be sure to have a comprehensive dilated eye exam at least once a year.
What is multiple sclerosis (MS)?
According to the National Multiple Sclerosis Society, MS is a chronic, unpredictable disease of the central nervous system (the brain, optic nerves, and spinal cord). It is thought to be an autoimmune disorder. This means the immune system incorrectly attacks the person’s healthy tissue.
Signs and Symptoms of Multiple Sclerosis
Symptoms of MS are unpredictable, vary from person to person, and from time to time in the same person. MS can cause blurred vision, loss of balance, poor coordination, slurred speech, tremors, numbness, extreme fatigue, problems with memory and concentration, paralysis, and blindness and more. These problems may be permanent or may come and go.
Most people are diagnosed between the ages of 20 and 50, although individuals as young as 2 and as old as 75 have developed it. Multiple sclerosis is not considered a fatal disease as the vast majority of people with it live a normal life-span. But they may struggle to live as productively as they desire, often facing increasing limitations.
What is traumatic brain injury (TBI)?
The National Institute of Neurological Disorders and Stroke say traumatic brain injury (TBI), a form of acquired brain injury, occurs when a sudden trauma causes damage to the brain. TBI can result when the head suddenly and violently hits an object, or when an object pierces the skull and enters brain tissue.
Signs and Symptoms of Traumatic Brain Injury
Symptoms of TBI can be mild, moderate, or severe, depending on the extent of the damage to the brain. A person with mild TBI may remain conscious or may experience a loss of consciousness for a few seconds or minutes. Other symptoms of mild TBI include headache, confusion, lightheadedness, dizziness, blurred vision or tired eyes, ringing in the ears, bad taste in the mouth, fatigue or lethargy, a change in sleep patterns, behavioral or mood changes, and trouble with memory, concentration, attention, or thinking. A person with a moderate or severe TBI may show these same symptoms, but may also have a headache that gets worse or does not go away, repeated vomiting or nausea, convulsions or seizures, an inability to awaken from sleep, dilation of one or both pupils of the eyes, slurred speech, weakness or numbness in the extremities, loss of coordination, and increased confusion, restlessness, or agitation.
Referenc es:
1. http://www.slideshare.net/wajihab/visual-impairment-45804251