Meibomian Gland scarring is due to a multifactorial process primarily due to:
1. Clogging of the orifice (ie, from makeup, Demodex mites/blepharitis, bacteria, dead cells, debris, inflammation, generally not cleaning eyelids or performing warm compresses)
2. Impaired Secretory Function of Gland/Lack of stimulation of the meibomian gland and orifice to pump out its oil [meibum] (ie due to decreased linking rates, electronic screen viewing decreases blink rates; drugs can decrease secretory function of glands)
3. Inflammation leading to internal and external (outside of the orifice from things like rosacea, chemicals, preservatives, diet choices)
4. Hormonal influences: from genetics, aging, drug use, level of exercise
5. Autoimmune factors that increase inflammation
6. Toxic external factors, like radiation, chemotherapy, drugs like Accutane
7. Trauma: external trauma like a laceration or lid surgery
Fibrous Tissue versus Keratinization:
Both fibrosis and keratinization are factors in meibomian gland scarring.
Keratinization is the process where the cytoplasm of the outermost cells of the epidermis (ie, your surface skin) is replaced by keratin (a fibrous protein that forms your epidermis [your surface skin], as well as nails, hoofs, claws, etc.).
Keratin is an important protein in the epidermis. Keratin has two main functions: to adhere cells to each other and to form a protective layer on the outside of the skin. In epithelial cells, keratin proteins inside the cell attach to proteins called desmosomes on the surface which keep cells together and make the skin waterproof.
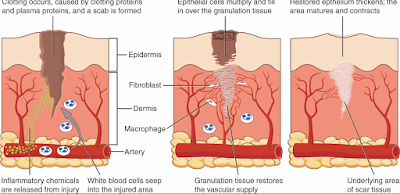
Fibrosis is the formation of excess fibrous connective tissue in an organ or tissue in a reparative or reactive process. Fibrosis is usually a result of inflammation shown below where fibroblasts are dumped in an area of inflammation and left there to heal the wound. Fibrosis results in a scar.
Does Meibomian Gland Probing Create Scar Tissue?
Meibomian Gland Probing is an attempt to break through kertinization and even fibrosis to restore the orifice and meibomian gland anatomy. The concern is that probing could lead to fibrosis and futher scar tissue but this has not been seen or reported yet. There are a couple of patients who I have seen who have had MGP multiple times by Dr. Maskin or myself who noted significant improvement after these treatments but then noted the MGP did not work as well. What may be happening is that the fibrosis that is being forced open during probing is continuing to take over the gland due to the underlying cause of the fibrosis (ie, rosacea, autoimmune disease, excessive electronic screen use, aging, etc). We know probing is not a cure for Meibomian Gland Disease but it significantly helps with pain relief for the majority of patients. I do not think MGP makes patients worse. I have seen many patients get significantly worse when nothing is done to save the meibomian glands.
References:
Abstract | April 2010
to Meibomian Gland Dysfunction (mgd)
Meibomian gland (MG) is an important and as yet underestimatedcomponent of the
functional anatomy of the ocular surface. Increasing evidence points to a high impact of
MG hyper-keratinisation as a major cause of obstructive MG
dysfunction (MGD) and evaporative dry eye disease. Information of the
normal keratinisation status and cytokeratin composition of the
human MG is limited.
whole-mount specimens including the lid margin from ten body donors were embedded
in paraffin. Serial sections were stained by H&E and
Masson-Goldners stain and by immunohistochemistry (IHC) with antibodies to
cytokeratins and related proteins.
conventional histology, the MG showed distinct similarities with the pilo-sebaceous unit of the
cilia. The keratinised skin epithelium extended into the
terminal part of the central duct and formed an excretory duct similar
to the opening of the hair follicle. Masson-Goldners stain of
tangential sections showedthat the whole ductal epithelium including the
connecting ductules contained keratohyalin granules in
the superficial epithelial cell layer. IHC staining showed that
the epithelium of the excretory duct, similar to the epidermis, was
strongly positive for the keratinisation marker CK10 which was
lost more proximal in the central duct. However, filaggrin, a
marker for incipient stages of keratinisation and located in
keratohyalin granules continued in the superficial layer of the duct
epithelium all along the normal Meibomian central ductal
system.
MG shares similarities with the cilia in embryology, in structure and in the cytokeratin
expression. It can hence be regarded as a “hair without a
hair shaft”. All parts of the normal MG ducts have signs of
incipient keratinisation and hence preserve a commitment to
keratinisation. Its upregulation in MGD explains hyper-keratinisation as
a typical event in obstructive MGD. A flow diagram is presented,
that summarizes the interacting events that form vicious circles in
obstructive MGD.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5914509/
Currently, there is no evidence
showing systemic medication induced MGD is due to inflammation. However, it was
suggested that systemic medication also could damage the gland or impair its
secretory function. We reported patients with loss of meibomian glands with
superficial punctate epitheliopathy during treatment of cancer with an
anticancer TS-1® combination capsules of tegafur, gimeracil, and
oteracil potassium (Taiho Pharmaceutical Co. Ltd, Japan) (Mizoguchi et al., 2015) (Fig.
2). The possible mechanism underlie TS-1®-related MGD might
be similar to the obstruction of drainage system or corneal epithelial disorders
associated with systemic TS-1, but not via direct toxicity of the drug to the
acinar cells. 5-FU leaked to tear fluid might cause local inflammation and
obstruction of the orifice of the gland. On the other hand, the influence of
inflammatory fibrotic diseases to the structure or function of meibomian glands
is to be further examined. Another case is long-standing consequences of
isotretinoin use. Without a significant finding in either gland or eyelid
margin the secretory function of these glands is impaired, causing dry eye
symptoms (Moy et al., 2015).