Here are the top 10 things you should know before getting cataract surgery:
1. Cataract surgery is generally medically necessary if the best vision or glare test is worse than 20/40 in the eye in question. In certain patients with Pseudoexfoliation (PXF) and/or previous trauma and/or glaucoma, most surgeons prefer to do cataract surgery sooner as it makes the surgery safer.
2. Your vision is composed of the Quantity & Quality of visual acuity:
Quantity can be improved by cataract surgery.
Quality depends on your meibomian gland function and your general tear film (ie you can prove this by not blinking for a few minutes –which Dr. Cremers does not recommend: your vision will get very blurry due to the evaporation of your tear film.
It is essential to know what your meibomian glands look like before any eye surgery so you will know how much discomfort you will have after (ie, due to dryness often) and the recovery time (ie a patient with significant meibomian gland loss may take longer to recover from vision & discomfort).
3. Femtosecond laser-assisted cataract surgery (FLACS) is the safest way to help remove the majority of cataracts. Some eyes cannot have FLACS due to advanced glaucoma, prior trauma, astigmatism issues.
4. Intraocular Implants: all implants have their positives and negatives. No one lens gives you perfect vision at all distances. It can be confusing but this is the one time where your eyeMD has the chance to try to get you glasses free for distance, intermediate, and/or reading, depending on your eye measurements.
a. Monofocal IOLs: are the only ones covered by insurance. It generally will only help with distance: either for reading, intermediate, or distance. If you have corneal astigmatism (the window of the eye is shaped like an American Football), you might need glasses for all distances (ie, progressives, 3 different pairs of glasses or trifocals-which most patients dislike).
b. Symfony Depth of Focus: is a patient favorite as it gives you good vision at 2 distances, usually distance and computer. But many will still need reading vision. Most patients love this implant but rarely a patient will be bothered by the glare.
c. Active Focus and Multifocals (Alcon & Tecnis): +2.5D Multifocal works well for better intermediate vision but some patients dislike the glare. Other Multifocal implants can help one eye see better for distance or reading but some patients really hate the glare after surgery (as this was the reason why they needed cataract surgery in the first place 🙁
d. Trifocals: approved in Europe. Not FDA approved yet in the US. Some patients still hate the glare. It does not achieve 100% happiness either, nor 100% 20/20 Uncorrected Distance visual acuity (UDVA):
-at 12 months post-surgery:
—76.2% had fully restored UDVA.
—39.8% had fully restored uncorrected intermediate visual acuity
— 22.6% had fully restored uncorrected near visual acuity.
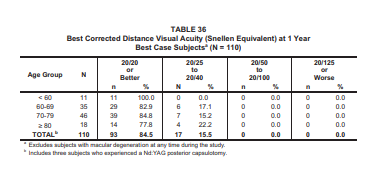
The FDA trials for Symfony did better with UDVA of overall 84.5% were 20/20 or better.
5. About 30% of patients need a YAG Capsulotomy with a YAG laser to open the posterior capsule after cataract surgery. It is considered part of the first surgery.
6. Most common issues/risks after cataract surgery are:
1. Need for glasses
2. Foreign body sensation usually due to an unstable tear film
3. Need for YAG capsulotomy
4. Glare/halos: usually improve with time.
5. Need for another surgery: this is uncommon. Causes: if there is a piece of cataract nucleus or cortex left; if the cornea decompensates and gets cloudy needing a DSEK or corneal transplant, IOL surprise (what the data said was the best IOL turns out to not be the best for the patient).
6. Other rarer risks: infection, loss of vision, loss of the eye, retinal detachment
7. If you have glaucoma ask your eyeMD about having a procedure at the time of Cataract Surgery to see if you can get off your glaucoma drops.
8. Sometimes the cataract is so dense, the eyeMD cannot tell if a patient had advanced macular degeneration and glaucoma. You will have to wait till after cataract surgery to determine what your best potential vision will be.
9. Diabetes & Diet & Keeping they eyelids clean: these go a long way to preventing vision issues after cataract surgery. Dr. Cremers recommends a low carbohydrate, low/no gluten or sugar diet as much as possible.
10. There are no guarantees with cataract surgery and it can be very frustrating to not have the vision you expected after cataract surgery. Thus it is very important to be sure your dry eye and diabetes is under control ideally before surgery.
I hope this helps you and your family.
SLC