What to Do For Headaches?
A patient asked me: I have had Headaches for over a week and they get worse every day. I’m on Topamax for migraines though. Also get dizzy randomly. Should I go to the Er for a CT? Don’t feel these are normal.
If you feel you are having the worst headache of your life, go to ER to a CT or MRI with contrast to be sure you do not have an aneurysm or tumor which is rare but can happen in totally healthy people.
Worsening headaches on Topamax, needs an evaluation for angle closure glaucoma by an eyeMD who has a Pentacam & is familiar with gonioscopy in such cases. Topamax can rarely (though I have personally seen 8 cases of this) cause angle closure glaucoma: see
So for mild-moderate headaches, I would recommend the following:
1. Change your diet while you wait to see your EyeMD or MD: see Migraine Diet post: https://drcremers.com/2014/02/migraine-diet-recommended-and-not.html
2. See EyeMD for:
a. good refraction
b. if you are younger than 40-45, ask for a cycloplegic refraction if you have a family history of accommodative spasm or if you have tried all options & your headaches persist. This dilated refraction will leave you dilated & unable to read & sensitive to the light for 1-3 days, but it may be worth it in some patients to see if they need a stronger glasses prescription to help their eye muscles not contract excessively and cause a headache/migraine.
c. Pentacam looking for narrow angle (see below) & Gonioscopy
d. Good dilated exam to look at optic nerve & retina to be sure there is no pallor of the optic nerve (which can signal glaucoma, or tumor pushing on the eye or brain).
e. Depending on symptoms & exam, we will do a Visual Field to look for any signs of issues in the brain.
f. If something of concern is found, your eyeMD will order a CT or MRI with contrast of the brain (& orbits in some cases).
3. See MD for a full exam & in particular a full neurologic exam, check blood pressure, HgA1C for diabetes, CBC to be sure all is ok with your general health. Sometimes Thyroid function tests help if you are having heat or cold intolerance, weight gain or loss, irritability.
4. If all is normal with your body & eye & neurologic exam & the diet (truly followed for at least 2 months) has not helped, then see neurologist for full neuro exam to see if a visual field is needed and/or a CT or MRI with contrast of the brain (& orbits in some cases).
5. As you wait for above appointments, start Migraine/Headache diary of when you notice pain, does pillow or position of neck at computer/desk make it worse. Start working on health of neck muscles & see if massaging or acupuncture type treatment helps relieve symptoms.
Treatments I use on myself for headaches: note this is a case study of 8 as this has helped my husband, kids, and some friends I taught it to, but it has never been studied in a randomized controlled study. So be aware there may be risks I have never heard about.
I personally find that if I find a headache starting, I massage my neck & shoulder muscles until I can feel the pain in my head getting worse & pinch those muscles till the pain is almost unbearable & then release it. I do this many times & it usually goes away. Also if the pain is above my eyes, I put pressure on the superior orbital notch until I feel the pain a bit more (about 3-5 seconds) and release. These two things usually take care of it. I would not recommend putting more than 5 seconds on pressure on the superior orbital notch as important blood vessels & nerves run through there, but no one I know has ever had a side effect with the above. In addition I make sure I am drinking 64oz or more of water & checking my sitting position so my neck muscles are not going to contract/spasm.
6. If you need ibuprofen (Advia) or acetaminophen (Tylenol), use it early into the headache. If you wait too long, many studies have showed, you will need more milligrams of the pain med to get your pain under control. This goes for all pain & pain meds to my knowledge.
7. If all else does not help and the MRI/CT is normal, then see your MD for a Rx for a stronger headache/migraine pill. See
Narrow Angle and risks of Acute Angle Closure Glaucoma with the Objective Measurements of the Pentacam
For many years both as a resident at New York Eye and Ear Infirmary and as an attending at Harvard Medical School, it never ceased to amazed us of how patients inevitably would come in to the ER with an acute attack of narrow angle glaucoma on a late Friday or Saturday night or middle of the night when the only doctor on call was a first year resident. Usually the first or second year resident would take care of these frightened patients so as not to “wake” the attending on call. Those of us who have taken care of these patients are often the ones who really look for narrow angles in our patients since we have seen the significant consequences narrow angle (a fully treatable condition that is often left untreated). Especially with so many drugs exacerbating narrow angles on the market these days (like sleeping pills, Benadryl, and TOPAMAX® (topiramate) ), there is a real need to warn these patients of the risk of having narrow angle.
However, since there are no symptoms with narrow angles often, except sometimes a mild headache, patients become suspicious when told they have something they have never heard of before. Who can blame them? Even after showing such patients their Pentacam (a more objective scan of their angle), some really are in disbelief.
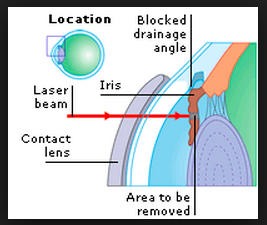
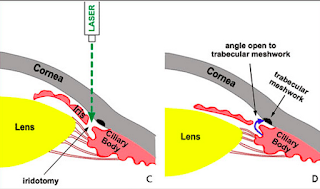
Recently a patient told me that she always got headaches every time she was dilated and could not understand why. When I told her it was from Narrow Angle she was surprised as she had never heard of this. When asked about family history she said no one in the family had any such history. Her Pentacam and Gonioscopy clearly demonstrated Narrow Angles. They were “occludable” in a dark room which means the iris tissue blocked off my view of the Trabecular Meshwork or Angle when the pupil dilated a bit and I was not pushing on the eye with the Gonioscopy contact lens instrument.
After her Laser Iridotomy, her chronic headaches went away and she never had a headache after dilation again. Interestingly, when she heard this was a genetic condition often, she went through her dad’s old medical records. She was shocked to see papers with the words “Narrow Angle” for her father and an appointment date for a Laser Iridotomy. Her dad never mentioned this to any of his kids or family.
Recently a patient told me that she always got headaches every time she was dilated and could not understand why. When I told her it was from Narrow Angle she was surprised as she had never heard of this. When asked about family history she said no one in the family had any such history. Her Pentacam and Gonioscopy clearly demonstrated Narrow Angles. They were “occludable” in a dark room which means the iris tissue blocked off my view of the Trabecular Meshwork or Angle when the pupil dilated a bit and I was not pushing on the eye with the Gonioscopy contact lens instrument.
After her Laser Iridotomy, her chronic headaches went away and she never had a headache after dilation again. Interestingly, when she heard this was a genetic condition often, she went through her dad’s old medical records. She was shocked to see papers with the words “Narrow Angle” for her father and an appointment date for a Laser Iridotomy. Her dad never mentioned this to any of his kids or family.
The below handout is given to all our patients with an Anterior Chamber Depth less than 2.5mm (the standard definition of narrow angle). There are so many factors that affect risks of acute angle closure, so it is hard to determine with 100% accuracy who will have an attack and who will not. Generally, most cases are not emergencies (unless the criteria are met below which are high risk).
But personally, if I had a narrow angle, knowing the minimal risk of having it treated with a laser that takes about 5-15min in general, and knowing the devastating consequences to my vision if an attack happens, I would have the laser done very soon.
NARROW ANGLES by Sandra Lora Cremers, MD, FACS
The angle of the eye is located between the cornea (the clear window of the eye) and the iris (the colored part of the eye) where fluid (aqueous) inside of the eye drains out to the trabecular meshwork or “sink.” Some people are born with narrow, drains/angles. Some develop increasing narrowing of the angle with age as the lens of the eye grows in circumference by adding rings like a tree. In people with narrow angles, this increase in circumference encroaches on the already limited anterior segment space. If left untreated, further narrowing of the angle can causes the pressure to build up and increase the risk of Acute Angle Closure (AAC) or Closed Angle Glaucoma which can cause sudden pain and blindness. Narrow angle can also cause glaucoma (slow but permanent optic nerve damage with vision loss) and causes almost half of the blindness from glaucoma. Be sure to check all medication inserts to look for precautions in patients with narrow angles. The best way to view the angle is with an instrument called a Gonioscopy. New technology allows us to perform measurements on the angle, though the gold standard remains gonioscopy (though there is more of a subjective assessment with this instrument since if an eyeMD pushes too hard, the angle may look “open” when in fact it is narrow.)
[If you would like to know more about risk: Objective measures from the Pentacam have helped quantify risk: ACV=anterior chamber volume; ACD=anterior chamber depth; ACA=anterior chamber angle; Standard Gonioscopy is more subjective.
|
Normal (approx)
|
Narrow Angle
|
High risk AAC Sensitivity
|
High risk AAC Specificity
|
|
ACV >171mm³
|
≤113 mm³ =88% sensitivity, specificity significant narrow angles (Shaffer grade ≤1)
|
≤100 µl 93.3%
|
≤100 µl 100%.
|
|
ACD >3.15mm
|
<2.5 mm
|
≤2.1 86.7%
|
≤2.1 100%
|
|
ACA >34°
|
>34°
|
≤26° 73.3%
|
≤26° 88.2%
|
There are 3 options to main options to treat Narrow Angles:
1. Observation: if the narrow angle is minimal or is not causing any symptoms (occasional headache, brow ache, blurry vision), the angle can we watched periodically with gonioscopy (a contact lens with 4 mirrors). There, however, is a risk of sudden loss of vision and angle closure. Most eye surgeons recommend laser iridotomy or lens removal soon to avoid this uncertain risk. Either way, be sure to return for repeat gonioscopy and tell your eye surgeon of headaches, brow aches, or vision changes, especially in the evening or after dilation (after dilation starts to wear off.)
2. Laser Peripheral Iridotomy (LPI): we use a laser to make a microscopic hole in the iris to help open the angle. LPI helps prevent angle closure. It can also delay the need for lens removal if there is no significant cataract. The biggest risk of LPI is that the hole closes over time and needs to be reopened (<5). The risk of transient intraocular pressure rise, persistent inflammation, hyphema, further cataract formation, endothelial cell loss, and scar formation is very low. LPIs should be done on both eyes but are usually not an emergency. It usually takes a few minutes per eye. We give a topical anesthetic to help with discomfort. Steroid drops are given four times a day for 2-3 days after the procedure to help decrease inflammation. Rarely, the laser iridotomy is not enough and a different type of treatment is needed (iridoplasty, iridectomy or lens removal).
3. Lens removal: This offers the advantage of improving the patient’s uncorrected vision and preventing further maturation of the lens (developing a hard cataract). Lens removal or cataract surgery decreases the risk of angle closure essentially to zero. The lens never grows back. This procedure has its own risks which can be further discussed with your eye surgeon. Lens removal is the best way to remove the risk of angle closure in most patients if needed.
Headaches and Migraines can present in different ways depending on a patient’s particular brain-flow pattern, internal and external conditions (e.g., general medical health, immunological condition, hormones, hydration, humidity). Pain in the head or even seeing bright or dark spots in vision without a headache or flashing lights with or without a headache (assuming vitreous and retinal exam is normal) can be due to an alteration in the blood flow to particular parts of the brain and represent a migraine or Ophthalmic Migraine.
Things YOU can do to help with your headache/migraine:
1. Keep headache/migraine diary: when is it really bad; when are your good days & why? Note: visual symptoms, dizziness, light sensitivity and look for any association with:
Headache and Migraine Diet
Sandra Lora Cremers, MD, FACS
Sandra Lora Cremers, MD, FACS
Headaches and Migraines can present in different ways depending on a patient’s particular brain-flow pattern, internal and external conditions (e.g., general medical health, immunological condition, hormones, hydration, humidity). Pain in the head or even seeing bright or dark spots in vision without a headache or flashing lights with or without a headache (assuming vitreous and retinal exam is normal) can be due to an alteration in the blood flow to particular parts of the brain and represent a migraine or Ophthalmic Migraine.
If the headache or migraine is new, changing patterns, only on 1 side of head, always in temple area, waking you from sleep, or getting worse or is not improved by any of these treatments, then see your MD AND eyeMD to do following:
1. Get a full refraction by an EyeMD: to be sure your headaches are not from eye strain: this is a very common cause of headaches
2. Request a Pentacam and Gonioscopy (if needed) to be sure headache is not due to Narrow angles which can cause headaches in some patients. I have had many patients tell me of their years of migraines and headaches, and multiple pill intake, which resolved after a low risk Laser Iridotomy procedure.
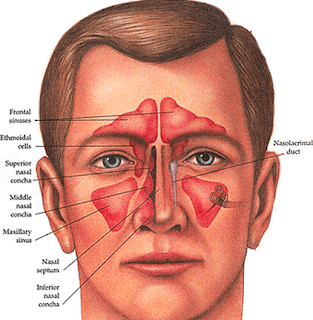
3. Check sinuses: first push on sinus are to see if it uncomfortable/painful: sometimes a CT with contrast or MRI is needed.
4. Request a full neurologic examination
If the eyes are fine and a general exam is normal, but you still have above symptoms, most primary MDs will recommend either a formal evaluation with a neurologist and/or a baseline brain scan (MRI or CT with contrast).
Things YOU can do to help with your headache/migraine:
1. Keep headache/migraine diary: when is it really bad; when are your good days & why? Note: visual symptoms, dizziness, light sensitivity and look for any association with:
1. Dehydration: are you drinking at least 64 oz of water per day. Dehydration is the #1 cause of headaches.
2. Gluten: if you can go gluten free for 2-3 months: did you notice any improvement in your symptoms?
3. Diet: avoid as many items on the list for at least 6 weeks: any improvement?
3a. Caffeine: too much or too little can set off a migraine: keep track of intake to see if associated with your headaches.
4. Stress & Anxiety: learn to pray and meditate and see if you can help control any pain from daily stresses.
4a. Push on your neck and shoulder muscles: do they hurt or are tender? Tense muscles in this area can cause tension headaches. Get a good massage to work out the “knots.” Find the pressure points that particularly hurt to see if you can “massage them out” gently.
5. Exercise: check with your general MD to be sure you can increase your exercise routine: any improvement or worsening with particular exercises?
6. Sleep: too little or too much can trigger headaches: find the best number of hours to sleep for you. For most people it is about 8 hours.
7. Weather patterns can be a factor: note the heat & humidity when you get a headache.
8. Heat: try to avoid extreme heat or cold: see which affects you more.
9. Light: especially fluorescent: avoid if affected
10. Loud Noise: some migraines are set off by this so make a note if so for you.
11. Hormonal changes: menstruation, ovulation, birth control pills can set off migraines: make a note
12. High Altitude
13. TMJ (Temporomandibular joint) pain or Teeth grinding: let your primary MD know & see a dentist.
2. Preventative Remedies: Over the counter:
1. Free: Prayer and Meditation. Learn to close your eyes and take deep breaths many times per day with thoughts or words with positive statements.
2. Drink plenty of water & follow migraine diet sheet to avoid triggers
3. Magnesium Dicitrate 600mg: Read Reference below prior to taking. Some literature says 400mg any form works for some people as well.
4. Vitamin B12 (Riboflavin; not just a B vitamin): 400mg/day; Read Reference below prior to taking.
5. Coenzyme Q10: 400 IU/day or is 100 mg three times per day. Read Reference below prior to taking.
6. Riboflavin: 400 mg per day; Read Reference below prior to taking.
7. Fish Oil at least 1200mg/day: for eyes or dry eyes, I recommend 2000-4000mg/day
8. Baby aspirin: coated: 81-325mg daily IF you have no history of allergy, stomach ulcers, rectal bleeding, GI issues.
9. Amitriptyline (or Nortriptyline) 25mg by mouth 3 times per day for insomnia and eye pain helps; they can make you drowsy: check with your primary MD before starting.
Sandra Lora Cremers, MD, FACS
References:
http://www.migrainetrust.org/assets/x/50129
Below: Modified from Dr. Katz’s Migraine Diet
Headache and Migraine Diet: Dietary Triggers
Food triggers do not necessarily contribute to migraines in all individuals, and particular foods may trigger attacks in certain people only on occasion. Be your own expert by keeping a journal of foods you have eaten before a migraine attack and see whether the removal or reduction of certain foods from your diet improves your headaches.
Skipping meals, fasting, and low blood sugar can also trigger migraines. If you are unable to follow a normal eating schedule, pack snacks.
—American Council for Headache Education
|
Food Type
|
Recommended
|
Not Recommended
|
|
Beverages
|
DRINK AT LEAST 64Oz WATER per day: most common cause of headache & migraines is DEHYDRATION.
Max 6oz/day decaffeinated coffee, Non-citric fruit juices, Max 4oz/day white wine. Herbal teas without citrus, club soda, non-cola soda (ex 7up, ginger ale, etc). Max 2oz/day vodka
White chocolate
|
Red wine, port, coffee, champagne, tea, iced tea, caffeinated sodas
Chocolate or cocoa
|
|
Breads and Cereals
|
Commercial breads: white, whole wheat, rye, French, Italian, English muffins, melba toast, crackers, rye, crisp, bagel
All hot and dry cereals: cream of wheat, wheaten, oatmeal, cornflakes, puffed rice and wheat
|
Avoid the following for sure, but I still recommend avoiding all gluten for at least 3 months and keeping a headache diary to see if this helps each patients:
Hot, fresh homemade yeast breads and crackers with cheese, croutons
Fresh yeast coffeecake, doughnuts, sour dough breads
Any breads containing chocolate or nuts
|
|
Dairy
|
Milk (2% or skim)
Cheese: American, cottage, farmers, ricotta, cream cheese, egg
Yogurt: limit to 4 oz per day
|
Some patients are particularly sensitive to dairy, others are note; there are some theories it may be related to blood type (but I have not seen any good studies to prove this yet);
Cultured dairy such as buttermilk, sour cream, chocolate milk
Cheese: blue, boursoult, brie types, camemberts, cheddar, swiss, gouda, Roquefort, stilton, mozzarella, parmesan, provolone, romano, and emmenlaler
|
|
Desserts
|
Sherberts, ice cream cakes and cookies without chocolate or yeast, Jell-O
|
All sugars increase inflammation so it is a good idea to avoid as much as possible:
Chocolate in ice cream, pudding, cookies, cakes |
|
Sweets
|
Sugar, jelly, jam, honey, hard candy
|
|
|
Food Type
|
Recommended
|
Not Recommended
|
|
Fruits
|
Any fruit juice such as prune, apple, cherry, apricot, peach, pear and fruit cocktail
Limit intake to ½ cup orange, grapefruit, tangerine, pineapple, raspberry, plums, raisins, papaya, passion fruit
|
Avocados, banana ( ½ allowed per day) lemon, lime
All nuts, peanut butter
|
|
Meat, Fish, and Poultry
|
Fresh or frozen turkey, chicken, fish, lamb, veal, pork, tuna
|
Aged, canned, cured, tenderized, processed meats, canned or aged ham, pickled herring, salted dried fish, chicken liver, aged game, hot dogs, sausage, bologna, salami, pepperoni, beef jerky, liver, any meal prepared with marinade
|
|
Sweets
|
Sugar, jelly, jam, honey, hard candy
|
|
|
Miscellaneous
|
Salt in moderation, lemon juice, butter or margarine, cooking oil, whipped cream, and white vinegar. Commercial salad dressings in small amounts as long as they don’t have additives to avoid
|
Migraine Triggers
“Triggers” are specific factors that may increase your risk of having a migraine attack. The migraine sufferer has inherited a sensitive nervous system that under certain circumstances can lead to migraine.
Triggers do not ‘cause’ migraine. Instead, they are thought to activate processes that cause migraine in people who are prone to the condition. A certain trigger will not induce a migraine in every person; and, in a single migraine sufferer, a trigger may not cause a migraine every time.
—American Council for Headache Education
|
Categories
|
Triggers
|
Examples
|
|
Dietary
|
Skipping meals/fasting
Specific foods
Medications
|
Overuse of over-the-counter medications can cause rebound headaches. Also, missed medication doses and certain medications (e.g. nitroglycerine, indomethacin) may cause headaches.
|
|
Sleep
|
Change in sleep patterns
|
Napping, oversleeping, too little sleep
|
|
Hormonal
|
Estrogen level changes and fluctuations
|
Menstrual cycles, birth control pills, hormone replacement therapies, peri-menopause, menopause, ovulation
|
|
Environmental
|
Weather
Bright Lights
Odors/Pollution
Other
|
Weather and temperature changes, extreme heat or cold, humidity, barometric pressure changes
Bright or glaring lights, fluorescent lighting, flashing lights or screens
Smog, smoke, perfumes, chemical odors
High altitude, airplane travel
|
|
Stress
|
Periods of high stress, including life changes
Accumulated stress
Reacting quickly and easily to stress
Repressed emotions
|
Factors related to stress include anxiety, worry, shock, depression, excitement, mental fatigue, loss and grief.
Both “bad stress” and “good stress” can be trigger (or prevent) migraines. Other triggers can include unrealistic timelines or expectations of oneself.
|
|
Physical
|
Overexertion
Injuries
Visual triggers
Becoming tired or fatigued
|
Over-exercising when out of shape, exercising in heat, marathon running
Eyestrain (if you wear glasses, make sure your prescription is current), bright or glaring lights, fluorescent lighting, flashing lights or computer screens
|