This article is from February 2012 and may contain outdated material.
During the past decade, the debate over the best approach to pterygium surgery has centered on whether surgeons should use sutures or fibrin glue to affix the conjunctival graft. Both approaches have their pros and cons in terms of such factors as surgical time, postoperative complications, cosmesis and recurrence.
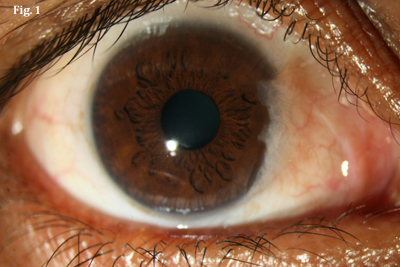
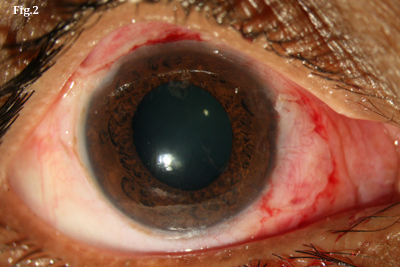
And now comes the latest twist: a novel approach in which the patient’s own blood is used for fixation (Figs. 1 and 2). Although it hasn’t been tested in a randomized, controlled trial, early results suggest that it may end up reshaping the debate altogether.
Sutures vs. Glue
Sutures. Conjunctival autografts using sutures are “the gold standard,” said Lawrence W. Hirst, MBBS. On the plus side, the grafts are stable, and the recurrence rate (approximately 15 percent) “has been the benchmark,” said Dr. Hirst, chief officer of Queensland Eye Institute in South Brisbane, Australia. As for the cosmetic result, it’s “acceptable but not wonderful,” he said.
On the minus side, the surgery itself can run 30 to 40 minutes, said Dr. Hirst, and suture-related problems include postoperative discomfort, chronic inflammation and granuloma formation.
Fibrin glue. Ophthalmologists have been using fibrin in a variety of surgeries, including lamellar corneal grafting and the closure of corneal perforations. More recently, the use of fibrin glue for suture-free conjunctival autografts has made significant inroads. “Glue is faster and simpler, and it works most of the time,” said Dr. Hirst. Surgical time is roughly half that of the traditional sutured approach, and patients report less postoperative pain and discomfort.
However, the glue itself is more expensive than sutures, and it can be difficult to obtain in some countries. And because fibrin glue is a blood-derived product, it carries the potential risk for transmission of viral and prion diseases. From Dr. Hirst’s perspective, the risk of disease transmission is mostly theoretical, however. “I don’t think that’s a major issue.” He is more concerned about the risk of dehiscence. “There’s a certain percentage of failure with glued grafts—not total dehiscence, but instances in which you’ve got to go in and fix something.”
What about recurrence? Theoretically, the rate should be lower with fibrin glue, given its ability to reduce inflammation. Nonetheless, the rate appears to be between 10 and 15 percent, Dr. Hirst said. “And no one has effectively assessed the cosmetic results with glue.”
Advantage: glue? In a meta-analysis published last year, the authors assert that fibrin glue is superior to sutures, as the glue results in a reduced risk of recurrence without an apparent increased risk of complications.1
Advantage: sutures? However, another approach, as developed by Dr. Hirst, has led some surgeons to favor sutures. In this technique, the excision, averaging 12 to 14 mm by 13 to 15 mm, is substantially larger than usual and involves extensive removal of Tenon’s layer (Fig. 3). “I do some reconstruction with the eye so that the suture lines are hidden,” said Dr. Hirst, who calls his procedure the “Pterygium Extended Removal Followed by Extended Conjunctival Transplant,” or P.E.R.F.E.C.T.
The procedure is a difficult and lengthy one, Dr. Hirst said, and patients experience a moderate amount of pain for 24 hours. “But there is virtually no recurrence and a good-looking eye.” He reported one recurrence in a series of 1,000 cases.2
|
|
 |
 |
|
(Fig. 1) Preoperative photograph shows pterygium impinging on the cornea. (Fig. 2)Same eye, two hours after graft fixation with autologous blood.
|
No Sutures, No Glue
The newest approach is autoblood graft fixation, a technique also known as suture- and glue-free autologous graft. Santanu Mitra, MBBS, presented study results with this method at the Academy’s Annual Meeting last fall.3
With traditional sutures, Dr. Mitra said, “the exaggerated symptoms of eye irritation—tearing, redness, foreign body sensation—in the postoperative period of grafting really inspired me to think of other approaches. The use of glue can take care of these problems, but the cost, availability and associated potential risks are constant problems.” In comparison, “Autologous blood is natural, has no extra cost or associated risks, and can overcome the postoperative irritations to a great extent,” said Dr. Mitra, who is a consultant at Disha Eye Hospitals in Kolkata, India.
How it works. With this approach, after the pterygium and associated conjunctiva are excised, the surgeon allows a thin film of blood clot to form over the bare area. Any active bleeding is stopped by direct tamponade. Next, a thin, Tenon-free conjunctival autograft, with or without inclusion of limbal stem cells, is fashioned. After the graft is aligned, it is placed over the blood film in the bare area, and the edges are held with forceps, usually for three to five minutes, to give adequate time for graft fixation to occur.
Results of two studies. In Dr. Mitra’s study—a prospective, noncomparative, interventional case series conducted in India—19 patients underwent autoblood graft fixation. Of these 19 patients, 17 had primary pterygia; two had recurrent pterygia. The mean surgical time was 11 minutes, no grafts were lost, and none of the pterygia recurred in the study’s six months of follow-up. Two patients experienced a medial edge recession, Dr. Mitra reported.
And in a cross-sectional study performed in the United Kingdom, 15 eyes (of 12 patients) received grafts affixed with autologous blood. The mean graft area was 24 mm2, the mean surgical time was 14 minutes, and the mean follow-up was 9.2 months. “Cosmesis was excellent in all cases, and visual acuity improved in one patient,” the researchers reported, and there were no intra- or postoperative complications requiring further treatment. No transplant dislocations or failures occurred.4
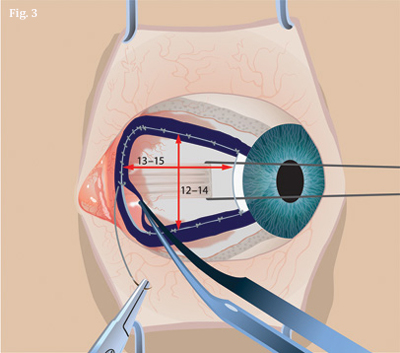 |
EXTENDED EXCISION.
Illustration shows final average size of conjunctival defect in P.E.R.F.E.C.T. technique. |
Fine Points to Consider
As with any new procedure, autoblood graft fixation involves a learning curve, said Jonathan E. Moore, FRCOphth, PhD, who participated in the U.K. study. “But this approach is probably less challenging [than sutures or glue] once one overcomes the fear of not suturing,” said Dr. Moore, a consultant ophthalmologist and clinical director at Cathedral Eye Clinic in Belfast, Northern Ireland.
He and Dr. Mitra noted several factors to consider.
Patient selection. Patients who regularly take aspirin or other blood thinners—or who suffer from a coagulation factor deficiency—would not be good candidates for autoblood graft fixation, Dr. Mitra said.
Surgical challenges. “You need a slightly oversized [about 0.5 mm] Tenon-free graft that is as thin as possible,” Dr. Mitra said. This prevents the risk of graft retraction and/or rejection. The surgeon will also need “a lot of patience,” he said, “giving more than adequate time—three to five minutes on average—during graft apposition.” Dr. Moore concurred with the need for thin grafts and “meticulous dissection to remove the Tenon’s layer” and cautioned, “Do not leave subgraft blood.”
Risk of dehiscence. “The main disadvantage is the risk of graft loss in the immediate postoperative period,” Dr. Mitra said. “But once the graft stays in place for the first 24 to 48 hours, it is going to stick around.” He added that he has seen no graft loss in his ongoing case series, which now numbers 63 patients who have been followed for at least one year.
Cosmetic results. “Cosmesis is excellent with this procedure—as good as with fibrin glue, if not better,” Dr. Moore said. “There is nothing to promote inflammation, and patients achieve a good appearance very quickly, within six weeks.” He added that the graft is not noticeable in many of his patients.
Risk of recurrence. If properly performed, the procedure appears to carry a low risk of recurrence. To date, Dr. Moore has performed 50 autoblood graft procedures, which have been followed for up to four years. None of his patients has experienced a recurrence. However, he reported, a surgeon in training at his institution used a graft that was too thick and did not cover the limbus, resulting in a small recurrence within the first two months following surgery.
Dr. Mitra reported one case of recurrence after the excision of a previously recurrent pterygium. “This probably was due to inadequate dissection of pterygial tissue rather than to autoblood fixation of the graft,” he said, and it was detected “just past the three-month postoperative follow-up examination.”
Visual outcomes. Although one of Dr. Moore’s patients experienced a two-line gain in VA, Drs. Moore and Mitra say that any effect on vision is independent of the graft fixation technique used. Instead, it will be influenced by factors such as the size and location of the pterygium, the presence of astigmatism, and other preoperative issues.
___________________________
Drs. Hirst, Mitra and Moore have no related financial interests, although Dr. Hirst owns the trademark “P.E.R.F.E.C.T. for Pterygium.”
___________________________
1 Pan HW et al. Ophthalmology. 2011;118(6):1049-1054.
2 Hirst LW. Extensive Incision and Conjunctival Transplantation for Pterygium: Results of 1,000 Surgeries. Presented at World Cornea Congress; April 7-9, 2010; Boston.
3 Mitra S et al. Autoblood as Tissue Adhesive for Conjunctival Autograft Fixation in Pterygium Surgery. Poster presented at the Annual Meeting of the American Academy of Ophthalmology; Oct. 22 and 23, 2011; Orlando, Fla.
4 de Wit D et al. Eye. 2010;24(9):1474-1477.
Do You Know Your Recurrence Rate?
Recurrence is “the bugbear” in pterygium surgery, said Dr. Hirst. “For patients, the No. 1 question is, ‘Will it come back?’ Everything else is secondary.”
And that should be the surgeon’s first question as well, he said. “If a pterygium comes back, it’s a real problem—it can be worse than the first occurrence. Yet many surgeons have no idea what their recurrence rate is.”
To get an accurate sense of recurrence—and, especially, to identify the earliest stages of recurrence—you need to follow patients for a full year, Dr. Hirst said. “That’s not a magical figure. If you want to pick up most of them, you’ll be able to do so within six months.” Still, you would miss a few if you stopped following patients at the six-month mark. “It’s a year if you really want to know what’s going on.”
|

