Key questions to ask your surgeon prior to making the decision:
1. Do I have a visually significant cataract?
A visually significant cataract is defined as documented lens protein changes noted on a microscope AND documented vision worse than 20/40 on exam or on glare test. When there are any concerns, the eye surgeon can take pictures of the cataract.
2. Do I have amblyopia?
(Amblyopia or “lazy eye” means one eye never developed the brain connection to see as well as the other eye or as good as 20/20 in childhood. This results in a chronic image blur from the “lazy eye” caused an inhibition of the visual signal to the bran. EyeMDs define amblyopia as a difference in vision of 2 or more lines between the eyes. For example, the good eye sees 20/20 and the “lazy eye” sees 20/30 or worse with the best glasses prescription before a cataract developed.
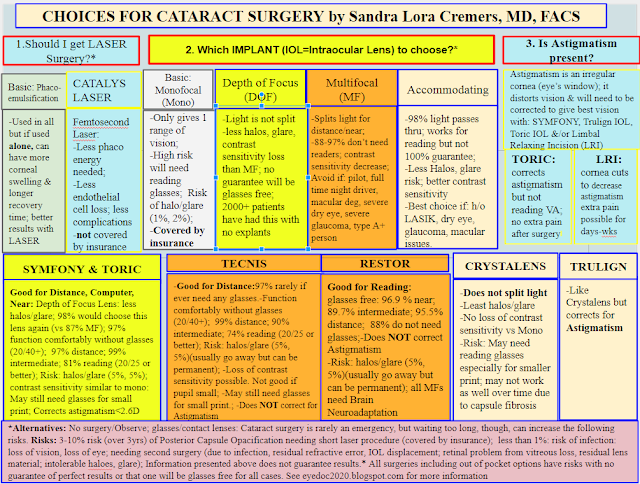
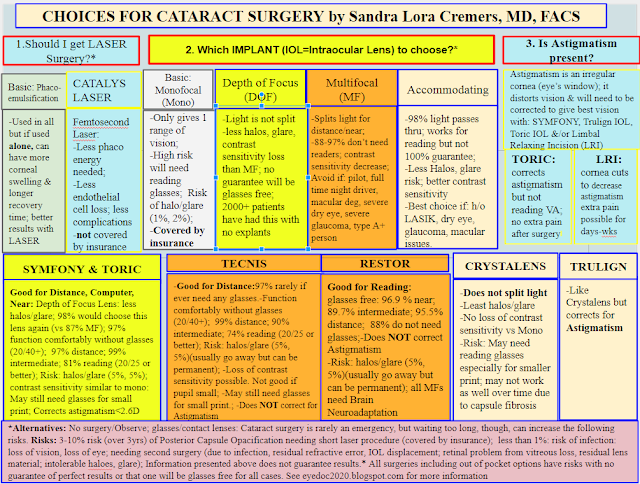
3. How much astigmatism do I have?
This determines what type of implant we should put in.
Astigmatism can come from the CORNEA (outer window of the eye) or LENS (inner usually clear structure behind the iris).
If the astigmatism comes from the cataract, we remove it with cataract surgery.
If the astigmatism comes from the cornea, we try to decrease as much of it as possible during the cataract surgery so as to minimize the need for glasses correction for this astigmatism. New innovative intraocular implants (IOLs) allow us to correct astigmatism better than in the past:
-Symfony Toric: The Symfony implant uses new technology to give patients an extended depth of focus. The Symfony Toric does an excellent job of correcting astigmatism and need for glasses in a range of options. It is not a 100% guarantee of begin glasses free for all distance for all situations, but it is the best we have thus far in the US as of 2018. Other options to correct astigmatism include:
-TORIC IOL: this is a monofocal platform that also corrects for astigmatism so it does not generally increase the risk of halos or glare after surgery the way Multifocoal implants can.
-Trulign IOL: works great to help decrease astigmatism but its ability to help relieve the need for glasses for distance, intermediate, reading can decrease over time.
-Restor Toric: This is a multifocal Toric IOL. It can increase your risk of haloes and glare after the surgery compared to Monofocal implants but not generally worse than the haloes and glare caused by the cataract in most cases. FDA approved and almost on the market as of December 20, 2014.
3. Do I have dry eyes?
Tearing, foreign body sensation, discomfort, rosacea are all associated with dry eyes.
Since the tear film is “like a pair of glasses” in that it is crucial in giving one good QUALITY vision, is very important to maximize one’s tear film prior to cataract surgery in order to give one the best change for high quality vision. See Lid hygiene instructions on blog.
https://drcremers.com/2018/05/best-way-to-treat-dry-eyes.html
4. Do I have a healthy eye to be able to be a candidate for the best surgical options in the world?
Some patients have macular issues, such as diabetic retinopathy or epiretinal membranes, or nerve problems, such as glaucoma or other nerve damage which limits their options for surgery.
5. What is my chance of needing glasses after surgery?
If your eye is a normal eye and you do not have irregular astigmatism AND you choose an advanced technology implant, research shows your chances of being glasses free is close to 81% for all distances options. For distance it is about 97% chance and for intermediate it is about 99%. It does not imply a guarantee for each patient but these large studies have showed good results with some of the best implants we have to date. If you choose a Monofocal implant, your chance of needing glasses for at least one distance is about 99% if the surgeon even if the surgeon specifically targets you to see without glasses for one focal plane (ie, one distance): the other distances (or focal planes) likely will be blurry without glasses.
6. What are my options if I have Amblyopia?
It used to be I would discourage all patients with amblyopia (or only one good eye) from choosing a multifocal implant (MIOL) for several reasons noted below on “Older Data.” New data shows that some patients with Amblyopia may benefit from new technology implants including multifocal implants.
Patients with amblyopia need to be warned of risks carefully and in particular told the following:
1. If you have true amblyopia, your vision will not be 20/20 after cataract surgery in most cases.
I have seen a patient who was told had amblyopia have 20/20 vision after cataract surgery because the patient’s other eye was 20/15+: so it was a relative amblyopia. At MEEI/Harvard I had 6 patients who were told they had amblyopia their whole lives only to be very surprised to find their vision in their “lazy eye” was not as “lazy” as they had thought and was only 1 line different compared to their good eye after successful cataract surgery.
2. If you have true amblyopia, protective glasses are recommended for your stronger eye. Still a couple of patients I have implanted an advanced technology lens are happy with the implant as their vision seems crisper in their “lazy eye,” even though they still need protective glasses.
7. Do I have glaucoma?
Glaucoma can be a blinding disease if not treated properly. We like to check patients’ anterior chambers to be sure there is no narrow angle if the patient has a cataract and wants to watch it and delay surgery. Chronic narrow angle is very common and a quiet killer of vision. If a patient has advanced glaucoma, a glaucoma procedure can be done at the time of cataract surgery to help decrease glaucoma drops or get them off the drops completely and save the vision long term from nerve damage. Severe glaucoma limits the ability to use Femtosecond laser in some cases: the risks of a dense cataract which may be decreased with the femtosecond laser may outweigh the risks of the pressure rise during Femtosecond laser. I know many surgeons who do use Femtosecond laser in glaucoma patients for this reason, but the long term effects on the optic nerve is still not know. Still the decreased risk of complications in the setting of a dense cataract makes Femtosecond laser an option even in patients with glaucoma.
Some key points are as follows:
1. Do NOT get a multifocal implant if: (as the halos & glare might be an issue)
a. If you drive at night a great deal.
b. Are a type A personality & notice all irregularities in your vision/health.
c. Have terrible dry eye (can make halos/glare worse).
d. Had previous RK/LASIK in the past and are NOT willing to have a touch up or IOL exchange if the multifocal implant bothers you: if you are willing to take this risk, many patients are finding they are happy with a multifocal implant even after LASIK surgery.
e. Have significant macular pathology (hole, epiretinal membrane).
2. Do NOT get a Crystalens if:
a. You absolutely do not want to wear reading glasses.
b. You have previously had a vitrectomy.
3. Do NOT get a MONOFOCAL lens if:
a. You absolutely do not want to wear reading glasses: unless you have told your eye surgeon you want to be corrected so you can see for reading without glasses (but then you will need computer vision and distance vision glasses.
Articles showing some patients with Amblyopia & Multifocals implants do well:
1. The implant below is not available in US yet but general principle indicates that some patients with amblyopia do well with innovative-technology implants.
References:
2018 Data:
Refractive lens exchange for a multifocal intraocular lens with a surface-embedded near section in mild to moderate anisometropic amblyopic patients.
Abstract
PURPOSE:
SETTING:
DESIGN:
METHODS:
RESULTS:
CONCLUSION:
Some key points are as follows:
1. Do NOT get a multifocal implant if: (as the halos & glare might be an issue)
a. If you drive at night a great deal.
b. Are a type A personality & notice all irregularities in your vision/health.
c. Have terrible dry eye (can make halos/glare worse).
d. Had previous RK/LASIK in the past and are NOT willing to have a touch up or IOL exchange if the multifocal implant bothers you: if you are willing to take this risk, many patients are finding they are happy with a multifocal implant even after LASIK surgery.
e. Have significant macular pathology (hole, epiretinal membrane).
2. Do NOT get a Crystalens if:
a. You absolutely do not want to wear reading glasses.
b. You have previously had a vitrectomy.
3. Do NOT get a MONOFOCAL lens if:
a. You absolutely do not want to wear reading glasses: unless you have told your eye surgeon you want to be corrected so you can see for reading without glasses (but then you will need computer vision and distance vision glasses.
Articles showing some patients with Amblyopia & Multifocals implants do well:
1. The implant below is not available in US yet but general principle indicates that some patients with amblyopia do well with innovative-technology implants.
References:
Through-Focus Optical Bench Performance of Extended Depth-of-Focus and Bifocal Intraocular Lenses Compared to a Monofocal Lens.
Abstract
PURPOSE:
METHODS:
RESULTS:
CONCLUSIONS:
Refractive lens exchange for a multifocal intraocular lens with a surface-embedded near section in mild to moderate anisometropic amblyopic patients.
Abstract
PURPOSE:
SETTING:
DESIGN:
METHODS:
RESULTS:
CONCLUSION:
Implantation of the multifocal ReSTOR apodised diffractive intraocular lens in adult anisometropic patients with mild to moderate amblyopia.
Abstract
AIM:
METHODS:
RESULTS:
CONCLUSION:
1st: in the FDA trial for the ReSTOR lens:
2nd: Patients with one good eye still should wear polycarbonate glasses for protection full time.
3rd: All eyeMDs try to avoid elective surgery in patients with only one good eye to avoid any undue risk. If a LASIK enhancement/adjustment is needed, or if you do not like multifocal vision, it could create a circumstance where additional surgery, such as an implant exchange, would be needed which again puts the eye at risk for complications, infections, loss of vision, loss of the eye, which though very rare are still present in most surgeries.
Have stated this, I have had many patients, though, who still wanted to have a multifocal implant or Crystalens implanted (many worked at the computer for many hours of the day and wanted to not have to have their glasses on at the computer) or did not have a severe amount of amblyopia and were willing to take the risk of not having glasses on the whole time. All these patients did very well but were very aware of the risks prior to making an informed consent. I do not have long term data on these patients, so I cannot say with certainty that their choice not to wear glasses full time was an issue long term.


