Below is a very good review of guidelines for COVID-10 care. My doctor friend said that hospitals are only admitting patients with less than 92% Oxygen Saturation and >60 breaths per minute (worse) with some exceptions..
In other words, if you are with someone that is sick, call your ER (if you can get through) to see if you should come in. If you are a health care provider or feel comfortable taking care of respiratory distress, I would recommend you buy a Pulse Oximeter especially if you have older parents or immunocompromised family members or anyone with respiratory issues.
My doctor friend recommended checking the pulse oximeter every hour in a family member in distress and to go to ER if any cyanosis (turning blue) or pulse oximeter is dropping below 95% knowing you may be turned back to go home if you do not meet criteria.
Below is a good revies of guidelines.
Not sneezing is not a presenting sign, so if you have sneezing, it is more likely allergy than COVID-19. Runny nose, though, has been added to list of presenting signs in some reviews I have seen but was not reported in the initial Lancet article below from China’s first cases.
No one knows if using Betadine/Iodine gargles & wiping the inside of the nose with Betadine/Iodine helps, but we have this ready in case we need to use it. We also have Cold Eeze (many packs).
I hope this helps.
SLC
References:
https://www.healthtap.com/blog/covid-19-care-guidelines/virtual-care-guidelines-for-covid-19?utm_campaign=COVID%20OUTREACH&utm_medium=email&_hsmi=84951814&_hsenc=p2ANqtz-8-6iUdmh-Fx7US07FP84f7FnxAukNATnckgN-0LMOUo2dj8ogc2Jv95c5UMjePWf4V_O9O&utm_content=84951814&utm_source=hs_email
MARCH 11, 2020
Virtual care guidelines: COVID-19
Guidelines for virtual care of patients with COVID-19 concerns
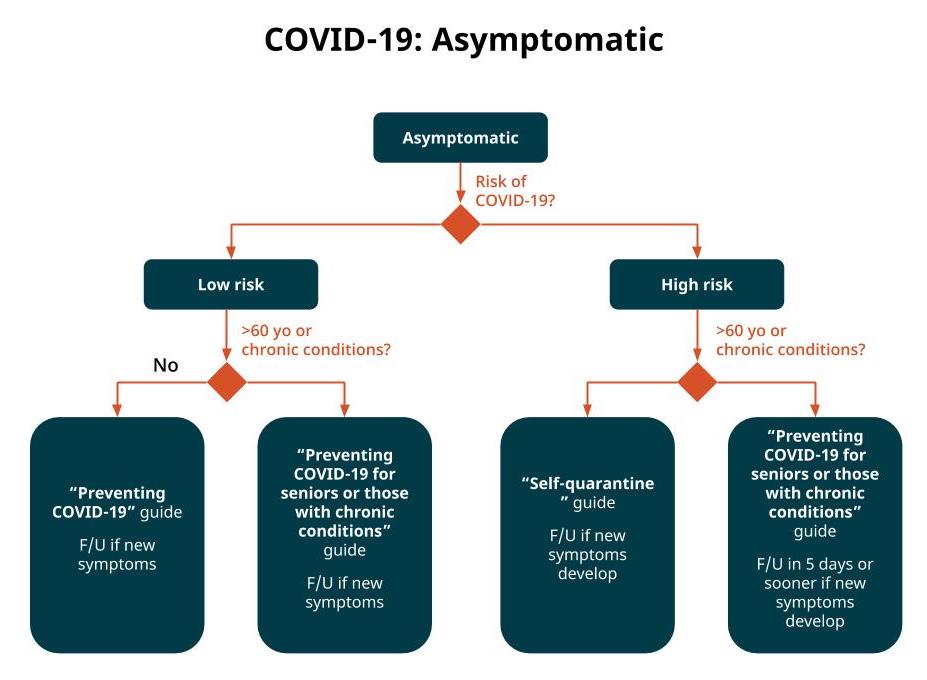
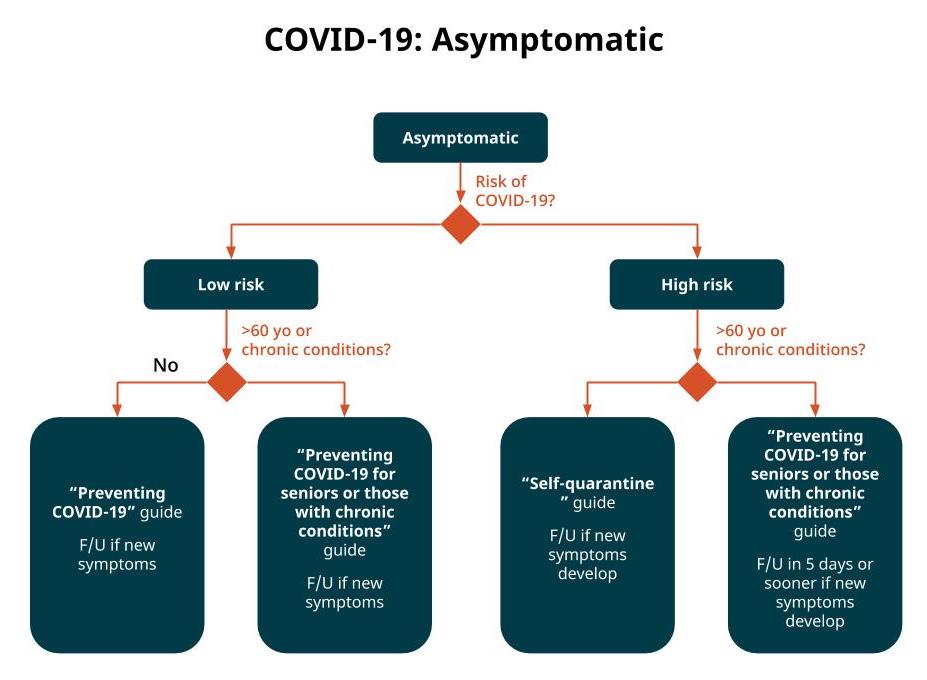
People who have no symptoms suggestive of COVID-19 should be given Healthy Living guidelines, plus if they are in a vulnerable group, they should be also given additional more restrictive guidelines to avoid contact with others:
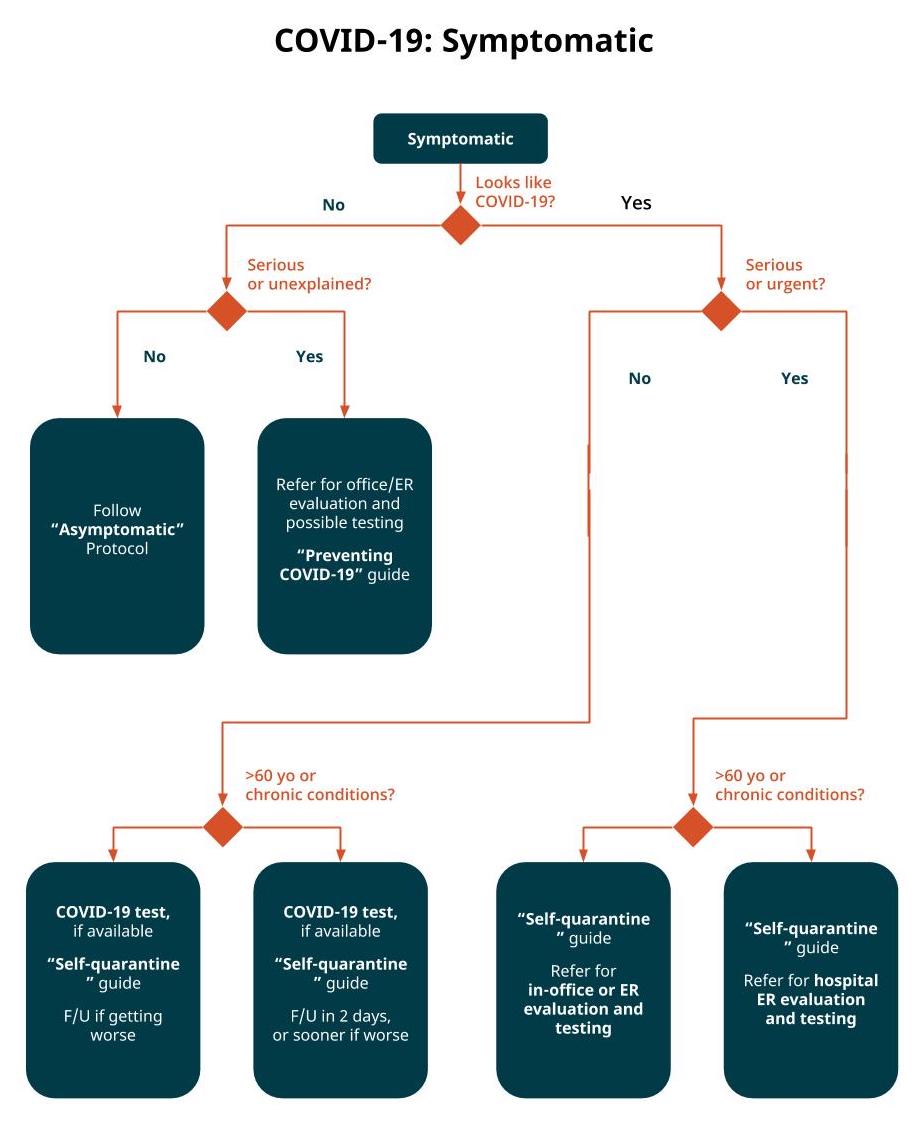
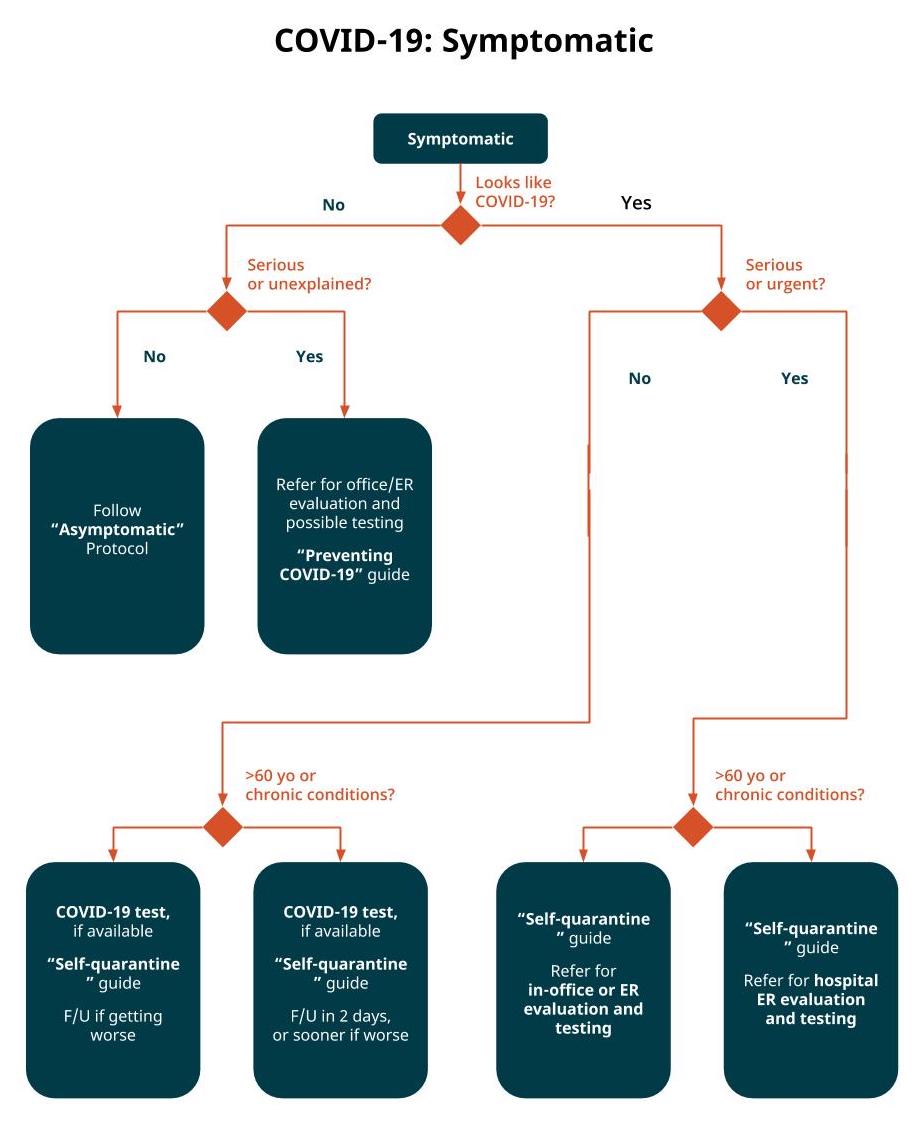
People who have symptoms compatible with COVID-19 who are in a vulnerable group (>60 yo and/or presence of an underlying medical condition) should be evaluated carefully and referred to the hospital if there are signs of significant pneumonia, or if relatively well, they can remain at home under self-quarantine with close daily or every-other-day followup via remote consultation. Low risk groups should be isolated at home with followup if symptoms worsen — with care ideally delivered via remote consultation. Be sure to order the COVID-19 test (SARS-CoV-2 PCR) for any patient you recommend to self-quarantine.
Evaluation during a virtual visit
Doctors who give virtual consults to patients regarding COVID-19 should evaluate:
-
Symptoms compatible with COVID-19
-
Risk of exposure to SARS-CoV-2 (based on region and travel history)
-
Vulnerability to complications from COVID-19 (based on age and medical conditions)
After evaluation, the diagnosis and treatment options should include some combination of:
-
Standard prevention guide for the young and healthy
-
Prevention guide for the more vulnerable
-
Self-quarantine guide (includes Guide for caregivers)
-
Get the COVID-19 test, if available without visiting the doctor’s office
-
Followup needed only if symptoms develop or worsen
-
Followup/check-in in 2 days or 5 days regardless
-
Refer to in-office doctor for evaluation and testing
-
Refer to hospital ER for evaluation and testing
-
Write an order for SARS-CoV-2 PCR (COVID-19) This will allow patients to obtain the test when available
Testing for COVID-19
Please include in your patient plan a doctor’s order for the COVID-19 test for any patient who has the presumptive diagnosis of COVID-19, by writing in your patient instructions:
“Lab order: SARS-CoV-2 PCR test”
Although tests for COVID-19 are not yet widely available, as testing sites open, patients will need a documentation of a doctor’s order for the test.
Symptoms of COVID-19
COVID-19 is a viral respiratory infection caused by the SARS-CoV-2 virus that may include lower and upper respiratory symptoms. A small proportion of cases may also include GI symptoms.
The most common symptoms presenting from COVID-19 (per NEJM article, patients in China Jan 29, 2020) include:
-
Cough (68%)
-
Fever (44%)
-
Fatigue (38%)
-
Body aches (15%)
-
Headache (14%)
-
Sore throat (14%)
-
Chills (12%)
-
Nasal congestion (5%)
-
Nausea, vomiting (5%)
-
Diarrhea (4%)
-
Tonsil enlargement or exudate (2%)
-
Eye itching or discharge (0.8%)
-
Glands swollen or tender (0.2%)
Risk of exposure to SARS-CoV-2
Assess the risk of exposure to this infection. Risk of exposure is high if the patient:
Otherwise the risk is low.
Vulnerability to COVID-19
Evaluate each patient to identify those who by age or presence of significant underlying medical condition are vulnerable.
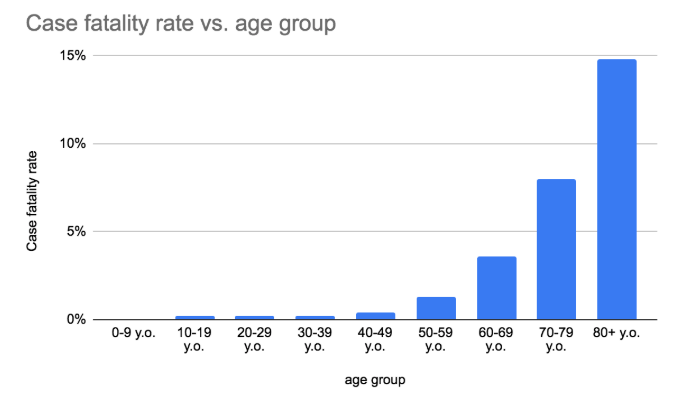
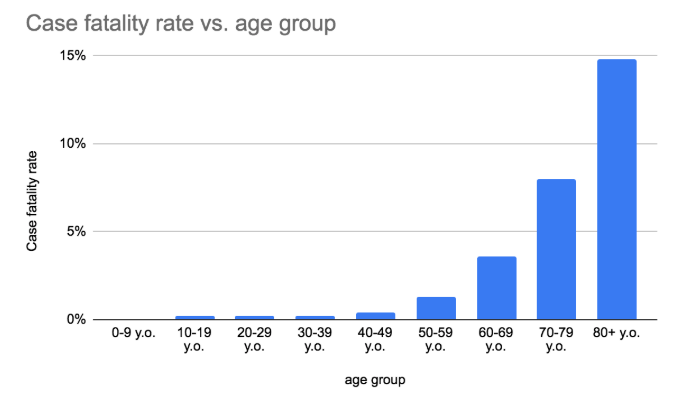
Most identified cases of COVID-19 are at low risk of death (~0.2%). Groups who are vulnerable (at higher risk of death) include those who have a significant underlying medical condition, and the elderly. The case fatality rate rises significantly for each year of age greater than 50. We consider a patient to be vulnerable if they are above age 65 or if below that age and have a significant underlying chronic medical condition.
-
-
Initial experience in China reports the case fatality rates for the following chronic medical conditions: Cardiovascular disease (10.5%), Diabetes (7.3%), Chronic respiratory disease (6.3%), Hypertension (6.0%) and Cancer (5.6%).
See the graphical protocols above for specific treatment recommendations. These are summarized as:
-
Asymptomatic/low risk of exposure/young & healthy
-
Asymptomatic/low risk of exposure/vulnerable
-
Asymptomatic/high risk of exposure/young & healthy
-
Asymptomatic/high risk of exposure/vulnerable
-
Symptomatic/not suspicious for COVID-19
-
Symptomatic/not suspicious for COVID-19 but unexplained symptoms/any age
-
Symptomatic/minor symptoms/young & healthy
-
Symptomatic/minor symptoms/vulnerable
-
Symptomatic/serious symptoms/young & healthy
-
Symptomatic/serious symptoms/vulnerable
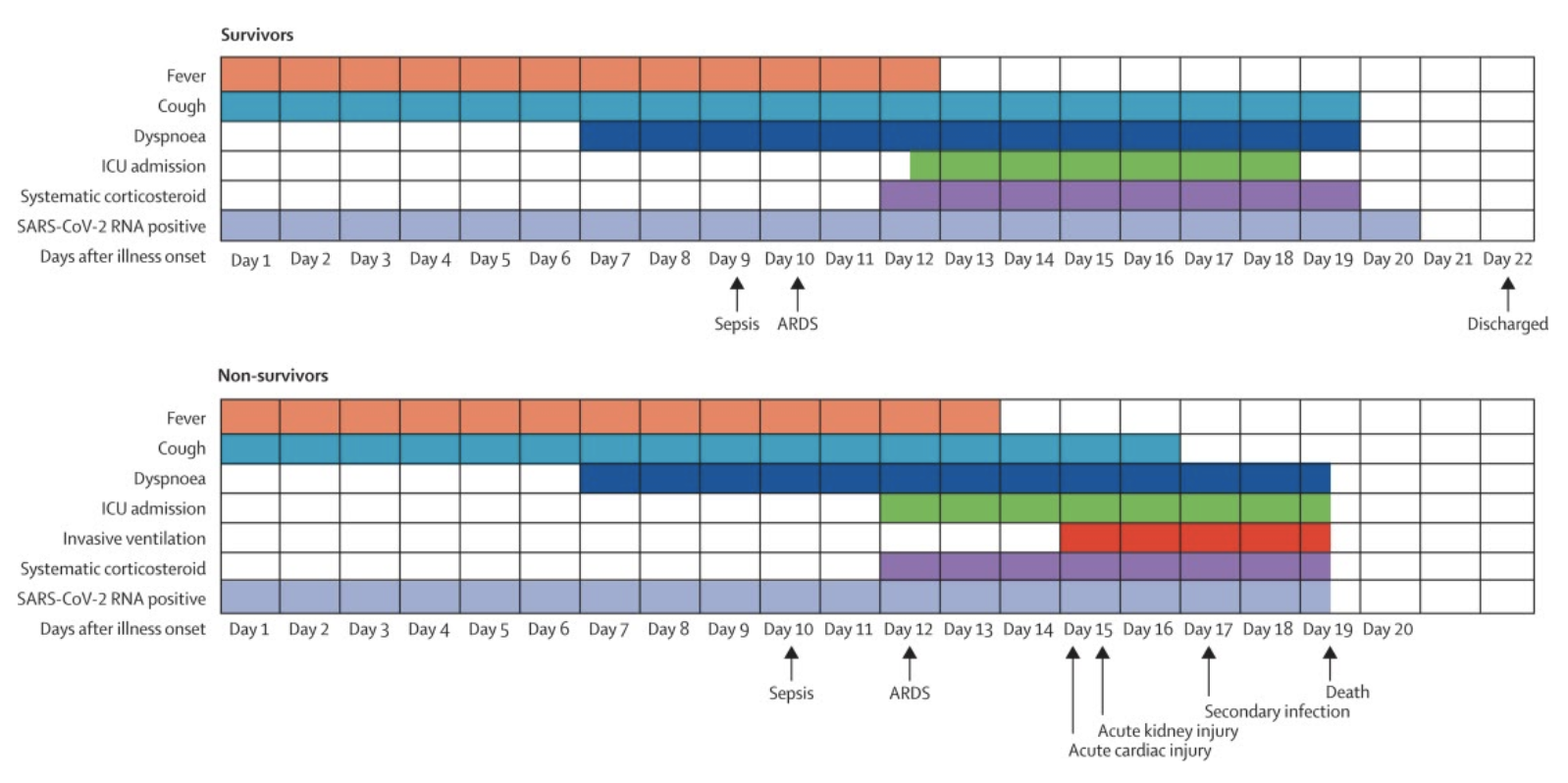
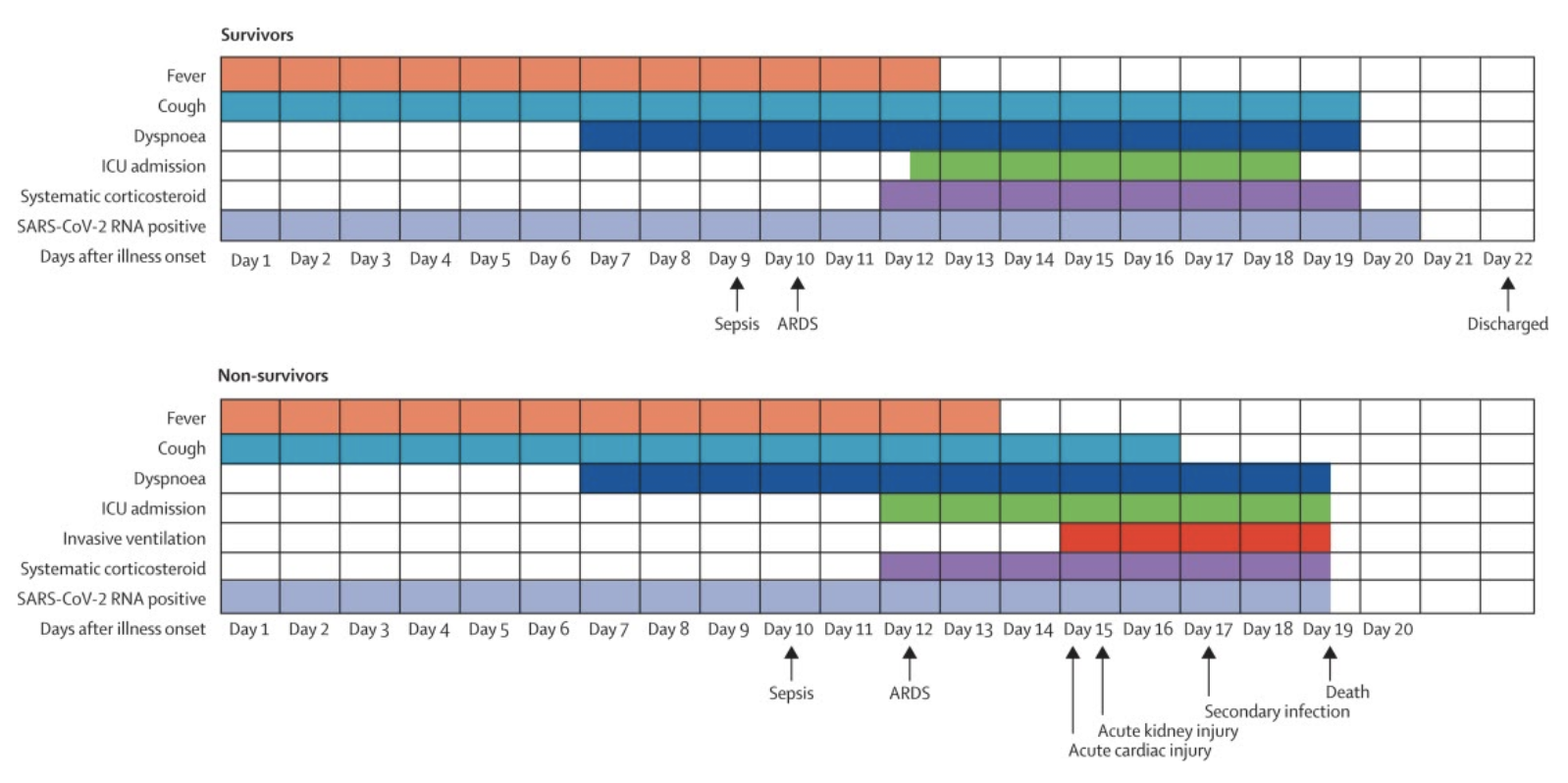
For reference, recent data published in
Lancet reveals the typical time course from illness onset for patients who were hospitalized:
References:
https://www.statnews.com/2020/03/03/who-is-getting-sick-and-how-sick-a-breakdown-of-coronavirus-risk-by-demographic-factors/
The new
coronavirus is not an equal-opportunity killer: Being elderly and having other illnesses, for instance, greatly increases the risk of dying from the disease the virus causes, Covid-19. It’s also possible being male could put you at increased risk.
For both medical and public health reasons, researchers want to figure out who’s most at risk of being infected and who’s most at risk of developing severe or even lethal illness. With that kind of information, clinicians would know whom to treat more aggressively, government officials would have a better idea of steps to take, and everyone would know whether they need to take special, additional precautions.
Here’s what research has shown three months into the outbreak:
Old and young
The vast majority of cases in China — 87% — were in people ages 30 to 79, the China Center for Disease Control
reported last month based on data from all 72,314 of those diagnosed with Covid-19 as of Feb. 11. That probably reflects something about biology more than lifestyle, such as being in frequent contact with other people. Teens and people in their 20s also encounter many others, at school and work and on public transit, yet they don’t seem to be contracting the disease at significant rates: Only 8.1% of cases were 20-somethings, 1.2% were teens, and 0.9% were 9 or younger. The World Health Organization mission to China found that 78% of the cases reported as of Feb. 20 were in people ages 30 to 69.
The death toll skews old even more strongly. Overall, China CDC found, 2.3% of confirmed cases died. But the fatality rate was 14.8% in people 80 or older, likely reflecting the presence of other diseases, a weaker immune system, or simply worse overall health. By contrast, the fatality rate was 1.3% in 50-somethings, 0.4% in 40-somethings, and 0.2% in people 10 to 39.
The age-related death risk probably reflects the strength, or weakness, of the respiratory system. About half of the 109 Covid-19 patients (ages 22 to 94) treated at Central Hospital of Wuhan, researchers there
reported, developed acute respiratory distress syndrome (ARDS), in which fluid builds up in the small air sacs of the lungs. That restricts how much air the lungs can take in, reducing the oxygen supply to vital organs, sometimes fatally; half of the ARDS patients died, compared to 9% of patients who did not develop the syndrome.
The ARDS patients had an average age of 61, compared to an average age of 49 for those who did not develop ARDS. Elderly patients “were more likely to develop ARDS,” the researchers wrote, suggesting how age can make Covid-19 more severe and even fatal: age increases the risk that the respiratory system will basically shut down under viral assault.
Youth, in contrast, seems to be protective. The WHO mission reported a relatively low incidence in people under 18, who made up only 2.4% of all reported cases. In fact, through mid-January, zero children in Wuhan, the epicenter of the outbreak, had contracted Covid-19. It’s not clear whether that’s because children do not show signs of illness even if infected.
Even cases among children and teens aged 10 to 19 are rare. As of Feb. 11 there were 549 cases in that age group, 1.2% of the total, China CDC found. Only one had died.
One intriguing explanation for the apparent resilience of youth: in regions near Hubei province, young children seem especially likely to be exposed to other
coronaviruses, scientists in China
reported in 2018. That might have given them at least partial immunity to this one.
Men and women
The effect of sex on susceptibility to Covid-19 is less clear than the age effect, but preliminary data suggest men might be more susceptible. China CDC found that 106 men had the disease for every 100 women, while the WHO mission found that men make up 51% of cases. A study of 1,099 Covid-19 patients in Wuhan through Jan. 29 found a greater imbalance: 58% were male, the China Medical Treatment Expert Group for Covid-19
reported last week in the New England Journal of Medicine.
It’s possible the apparent sex imbalance reflects patterns of travel and contacts that make men more likely to be exposed to carriers of the virus, not any inherent biological differences. It’s also possible the apparent worse disease severity in men could skew the data. Among hospitalized patients, there is “a slight predominance of men,” U.S. researchers
wrote last week in JAMA. If the virus hits men harder than women, health care systems will see, test, and count more men.
To determine if there are sex differences in susceptibility to infection would require an unethical experiment: expose 1,000 otherwise similar men and women to the virus and see who gets sick.
The difference is fatality rates, however, is real: 1.7% for women and 2.8% for men, China CDC reported.
Sick or healthy
The male-female difference in fatality rates, and perhaps in reported incidence, may arise from differences in underlying health. People with pre-existing illness are more likely to get seriously ill from Covid-19, and men have a higher incidence of such chronic illnesses as cardiovascular disease.
In the first large
study of the effect of underlying illness, researchers in China analyzed 1,590 patients from throughout the country with laboratory-confirmed disease. They calculated how “co-morbidities” — existing illnesses — affected the risk of being admitted to intensive care, being put on a ventilator, or dying.
After taking into account the patients’ ages and smoking status, the researchers found that the 399 patients with at least one additional disease (including cardiovascular diseases, diabetes, hepatitis B, chronic obstructive pulmonary disease, chronic kidney diseases, and cancer) had a 79% greater chance of requiring intensive care or a respirator or both, or of dying, they reported last week in a paper posted to medRxiv, a preprint site that posts research before it has been peer-reviewed. The 130 with two or more additional diseases had 2.5 times the risk of any of those outcomes.
That fits with what’s known about other respiratory viruses. People with a single co-morbidity who catch avian flu (H7N9) are 3.4 times more likely than otherwise-healthy flu patients to require ventilators and other intensive care. SARS and MERS, which are also caused by coronaviruses, are more severe in patients with underlying illnesses, too.
Breaking down the Covid-19 risk with the most common co-morbidities, the scientists found that cancer raises the risk 3.5-fold, COPD 2.6-fold, and diabetes and hypertension by about 60%. Because it isn’t unusual for someone to have an underlying disease (especially diabetes and hypertension) but not know it, the last figure is likely an underestimate.
Co-morbidities also raise the risk of dying from Covid-19. China CDC’s analysis of 44,672 patients found that the fatality rate in patients who reported no other health conditions was 0.9%. It was 10.5% for those with cardiovascular disease, 7.3% for those with diabetes, 6.3% for people with chronic respiratory diseases such as COPD, 6.0% for people with hypertension, and 5.6% for those with cancer.
Underlying disease might change the course of Covid-19. During the height of the epidemic in Wuhan, 37 of 230 patients receiving dialysis for kidney failure at Renmin Hospital developed the disease. Even though none were sick enough to require intensive care or a mechanical ventilator, six of them died, for a very high fatality rate of 16%. Oddly, however, none of the six died of pneumonia, Renmin researchers
reported. Instead, the causes of death were heart disease, stroke, and high blood levels of potassium (a result of kidney failure). The high fatality rate of Covid-19 in already-sick people might result not from the virus but from an exacerbation of existing disease.
About 60% of U.S. adults have at least one underlying health condition, Tom Frieden, former director of the U.S. Centers for Disease Control and Prevention, told reporters on Monday.
Pregnancy
In early February, Chinese state media
reported that a woman infected with the virus gave birth to a baby who later tested positive for it. Newborns might become infected because of close proximity to a patient, like anyone else, but the case raised fears that a pregnant woman can transmit the virus to her fetus via the placenta.
Only one small study has investigated such “vertical transmission.” Scientists at Wuhan University
found that, of nine pregnant patients infected with the virus (all had a caesarean section) in their third trimester, none seemed to pass the virus to their babies, all of whom scored at the top of the Apgar scale of newborn health.
As for the mothers, “Covid-19 seems not to be especially severe in pregnant women, at least based on the small number in this study,” the scientists wrote. That was somewhat surprising because pregnancy suppresses the immune system (so it doesn’t attack the fetus); pregnant women are more susceptible to respiratory pathogens than non-pregnant women. Nevertheless, none of the nine women developed severe Covid-19 pneumonia.
It may be that immuno-suppression is actually helpful. Some of the most serious symptoms of Covid-19 result from an immune system on the rampage rather than a lethargic one, Chinese scientists
found: An extreme immune response called cytokine storm, a flood of immune cells and the biochemicals they produce, tears through lung tissue.
Cytokine Storm: is thought to be a keye reason of why so many died with the Spanish Flu
chemopreventive agents such as
EGCG from green tea, myricetin, quercetin, 5-deoxykaempferol, 6-gingerol, and resveratrol, all isolated from
fruits and vegetables, which are able to prevent skin carcinogenesis
New therapies for the treatment of cystic fibrosis
patients are emerging during the last years. Pr. Roberto
Gambari (Department of Biochemistry and Molecular
Biology, Italy) reported the extraction of two natural
products citropten and bergapten from bergamot, which
expressed a high inhibition potential against the expression
of IL-8; NF-jB plays a key role in IL-8 expression. Furthermore, the investigation into a furocoumarin database
led to the discovery of furo(3,2-c)chromen-4-one derivative, which could be a potential pharmaceutical drug to
control lung inflammation in CF patients.
Pr. Bharat Aggarwal (Department of
Many phytochemicals—such
as the organosulfur compound sulforaphane, the polyphenol curcumin and the sesquiterpene zerumbone—
exerted antioxidant gene expression, by oxidation or
covalent modification of thiol groups associated with the
presented transcription factors and in this way maintain
cellular homeostasis. Though, these mentioned molecules
play a crucial role in chemoprevention and cytoprotection