|
Autologous Platelet-Rich Plasma, PRP, has been used for years in many fields of medicine and surgery to help heal damaged and scarred tissues. PRP is obtained by centrifuging one’s own blood to separate the platelets from the rest of the whole blood. PRP works due to the upregulation of growth factors and cytokines contained in platelet alpha granules. PRP has been used for the injection into joints, for faster healing of severe ulcers and burns, as well as for use in hair loss and cosmetic treatments. Recently, physicians and cosmetologists across the world have been using PRP as cosmetic filler for skin shaping and “healing.” Many cosmetic surgeons and cosmetologists mix the PRP with other fillers. This can be very dangerous as the case below illustrates.
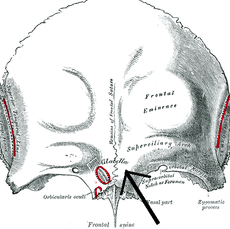
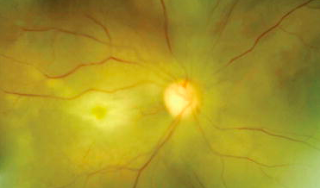
The below case is the first reported case in the world of vision loss (in her right eye) after PRP was injected into the wrinkles of her glabellar area (black arrow below shows location). The needle was large and was inserted deeper on her right side compared to her left side per the patient who is 49yo. |
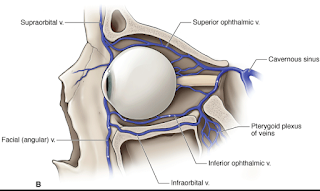
The cosmetologist was unlicensed and the patient refused to tell the treating doctors who did the procedure so some facts are unknown. Likely the PRP was mixed with fillers and the cosmetologist went subdermal (ie too deep) and pushed the PRP into the ophthalmic artery and vein area (see below at end if would like to see exactly where this likely happened: warning–anatomy photos are unpleasant).
I do not believe this would happen with PRP insertion into the Meibomian Glands for the below reasons. However, there is no 100% guarantee of such a complication with any procedure involving PRP. Of note, the complication of vision loss and even stroke, have been reported with steroid injections, epinephrine injections, fat injections into the skin area in many different locations, not necessarily into the eye or even just around the eye. All of these cases to my knowledge involved a large bore needle, not a 150 micron needle or cannula.
PRP insertion into the glands is likely very safe for the following reasons:
1. Inserting PRP into the glands involves insertion into an avascular orifice. During probing there might be a little blood due to scar tissue presence but usually that is minimal if at all present. There are blood vessels around the glands but not in the gland usually.
2. A 150-micron (150 µm) cannula is used and the ability of such a small cannula to force PRP into a blood vessel is very unlikely. The case below used a large bore needle which likely did penetrate a blood vessel.
3. 100% PRP is used. No fillers are added.
4. No complication of PRP into Meibomian Glands has been reported to date.
5. Only surgeons insert PRP into the glands.
Still, it is important to understand every procedure does have risks.
SLC
Irreversible Blindness Following Periocular Autologous Platelet-Rich Plasma Skin Rejuvenation Treatment
Kalyam, Krishnapriya M.D.; Kavoussi, Shaheen C. M.D.; Ehrlich, Michael M.D.; Teng, Christopher C. M.D.; Chadha, Nisha M.D.; Khodadadeh, Sarah M.D.; Liu, Ji M.D.
Department of Ophthalmology and Visual Science, Yale Eye Center, Yale University School of Medicine, New Haven, Connecticut, U.S.A.
Accepted for publication February 1, 2016.
Drs. Kalyam and Kavoussi are co-first authors with equal contributions.
The authors have no financial or conflicts of interest to disclose.
Address correspondence and reprint requests to Ji Liu, M.D., Department of Ophthalmology and Visual Science, Yale Eye Center, Yale University School of Medicine, 40 Temple Street, Suite 1B, New Haven, CT 06510. E-mail:liu.ji@yale.edu