Key Points
Question For patients with eyes having diabetic macular edema involving the macular center and vision 20/25 or better, what is the effect on vision loss of initial management with aflibercept vs laser photocoagulation vs observation, with aflibercept added to laser photocoagulation and observation if vision worsens?
Findings In this randomized clinical trial of 702 eyes, a 5-letter or more decrease in visual acuity at 2 years was not significantly different between groups initially managed with aflibercept (16%), laser photocoagulation (17%), and observation (19%).
Meaning Among eyes with diabetic macular edema involving the macular center and good visual acuity, there was no significant difference in vision loss at 2 years whether eyes were initially managed with aflibercept, laser photocoagulation, or observation.
Importance Intravitreous injections of antivascular endothelial growth factor agents are effective for treating diabetic macular edema (DME) involving the center of the macula (center-involved DME [CI-DME]) with visual acuity impairment (20/32 or worse). The best approach to treating patients with CI-DME and good visual acuity (20/25 or better) is unknown.
Objective To compare vision loss at 2 years among eyes initially managed with aflibercept, laser photocoagulation, or observation.
Design, Setting, and Participants Randomized clinical trial conducted at 91 US and Canadian sites among 702 adults with type 1 or type 2 diabetes. Participants had 1 study eye with CI-DME and visual acuity of 20/25 or better. The first participant was randomized on November 8, 2013, and the final date of follow-up was September 11, 2018.
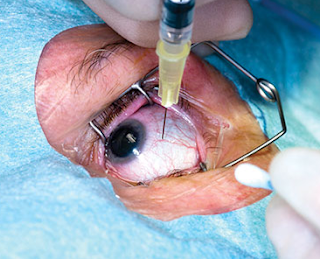
Interventions Eyes were randomly assigned to 2.0 mg of intravitreous aflibercept (n = 226) as frequently as every 4 weeks, focal/grid laser photocoagulation (n = 240), or observation (n = 236). Aflibercept was required for eyes in the laser photocoagulation or observation groups that had decreased visual acuity from baseline by at least 10 letters (≥ 2 lines on an eye chart) at any visit or by 5 to 9 letters (1-2 lines) at 2 consecutive visits.
Main Outcomes and Measures The primary outcome was at least a 5-letter visual acuity decrease from baseline at 2 years. Antiplatelet Trialists’ Collaboration adverse events (defined as myocardial infarction, stroke, or vascular or unknown death) were reported.
Results Among 702 randomized participants (mean age, 59 years; 38% female [n=264]), 625 of 681 (92% excluding deaths) completed the 2-year visit. For eyes with visual acuity that decreased from baseline, aflibercept was initiated in 25% (60/240) and 34% (80/326) in the laser photocoagulation and observation groups, respectively. At 2 years, the percentage of eyes with at least a 5-letter visual acuity decrease was 16% (33/205), 17% (36/212), and 19% (39/208) in the aflibercept, laser photocoagulation, and observation groups, respectively (aflibercept vs laser photocoagulation risk difference, −2% [95% CI, −9% to 5%]; relative risk, 0.88 [95% CI, 0.57-1.35; P = .79]; aflibercept vs observation risk difference, −3% [95% CI, −11% to 4%]; relative risk, 0.83 [95% CI, 0.55-1.27; P = .79]; laser photocoagulation vs observation risk difference, −1% [95% CI, −9% to 6%]; relative risk, 0.95 [95% CI, 0.64-1.41; P = .79]). Antiplatelet Trialists’ Collaboration vascular events occurred in 15 (7%), 13 (5%), and 8 (3%) participants in the aflibercept, laser photocoagulation, and observation groups.
Conclusions and Relevance Among eyes with CI-DME and good visual acuity, there was no significant difference in vision loss at 2 years whether eyes were initially managed with aflibercept or with laser photocoagulation or observation and given aflibercept only if visual acuity worsened. Observation without treatment unless visual acuity worsens may be a reasonable strategy for CI-DME.