LASIK is NOT 100% safe.
Patients has been complaining for years about their dry eye symptoms and corneal aberration issues, such as burning, tearing, pain, halos, and glare after LASIK. Not everyone who gets LASIK has dry eyes or corneal aberration issues afterwards, but it has been estimated that about 95-97% of patients get some form of dry eye immediately after LASIK (Ref 1), 60% of patients 1 month post-surgery, and 10%–40% of patients have chronic (lasts at least 6 months) dry eye after LASIK or PRK (Ref 2-4). Studies have also shown the risk of immediate dry eye and chronic dry eye after PRK is not less than LASIK.
More and more patients are noting the despair they feel from chronic dry eye after LASIK/PRK.
A recent New York Times article highlights this https://mobile.nytimes.com/2018/06/11/well/lasik-complications-vision.html
The recent March For Our Eyes – Lasik Protest In DC on 13 April 2018 also highlights the devastation LASIK and PRK can cause.
Who is at risk of getting severe dry eyes after LASIK/PRK?
1. If you have an abnormal meibography, do not get LASIK/PRK. Be sure to ask for a meibography before any refractive or cataract surgery.
2. Autoimmune disease: if you have an underlying autoimmune disease, you are more at risk. Autoimmune disease should be a contraindication for LASIK/PRK.
3. History of Accutane: As Accutane can destroy meibomian glands, be sure you have normal meibomian glands before having any refractive surgery. My recommendation is to not have LASIK/PRK anyway unless really need it for work and especially to avoid if you had Accutane in the past.
4. Computer programmers or people who use electronic screens more than 4-6hrs per day. My hypothesis is that people do not blink as often on screens (this is known but its conclusion has not been proven yet), which leads to less milking of the meibomian oil gland, which leads to an abnormal tear film and possible chronic dry eye. If you are a computer programmer, do not get LASIK/PRK.
5. Other risk for getting visual aberrations after LASIK/PRK:
– large pupils; thin corneas,
-abnormally shaped corneas or other corneal abnormalities or scarring;
-high degrees of astigmatism;
-severe dry eye; and possibly people who have other
-patients who have other sensitivities, pain syndromes or neurological disorders, frequent headaches or anxiety and depression.
Detailed Risks after LASIK/PRK:
1. Approximately 700,000 LASIK cases were performed in 2017, up from 628,724 in 2016, according to Market Scope, a market research company that focuses on the ophthalmic industry.
2. Both acute and long–term ocular pain and discomfort following LASIK have been reported [6,14,15]. It is suggested that almost all patients have at least mild symptoms after their procedure and that 20-55% of patients have persistent symptoms, defined as symptoms at 6 months or more post-procedure
3. Researchers at Ohio State University analyzed clinical data submitted to the F.D.A. by Lasik system manufacturers. The researchers reported in 2007 that while most of the roughly 4,500 patients had achieved 20/20 or 20/40 vision six months after the procedure, 20 percent had dry eyes that were severe or worse than before surgery.
4. 20 percent and 55 percent of Lasik patients have persistent dry eyes, defined as lasting at least six months after surgery (reference below: Galor et.al.).
| Study | Procedure | N | Design | Definition | Incidence |
|---|---|---|---|---|---|
| Denoyer 2014 [18] | LASIK | 60 | Prospective series | Use of eye drops at 6 months | 43% |
| De Paiva 2006 [19] | LASIK | 35 | Prospective randomized (nasal vs. superior hinge) | Fluorescein staining score of 3 or more at 6 months | 36.4% (overall) |
| Shoja 2007 [14] | LASIK | 95 | Retrospective series | Subjective symptoms at 6 months | 20% |
| Donnenfeld 2003 [20] | LASIK | 52 | Prospective randomized (nasal vs. superior hinge) | Patients reporting eyes drier than before LASIK at 6 months | 31% (overall) |
| Tuisku 2007 [13] | LASIK | 20 cases | Retrospective case-control | Subjective symptoms at 2 – 5 years |
55% |
| Hovanesian 2001 [16] | LASIK and PRK | 781 | Mailed questionnaire | Subjective symptoms at 6 months or more | 44% |
https://www.ncbi.nlm.nih.gov/pubmed/25896684
Treatment Options:
There are many treatment options for Dry Eye Symptoms in general and particularly after LASIK. Some surgeons routinely place punctal plugs before LASIK is done or shortly thereafter.

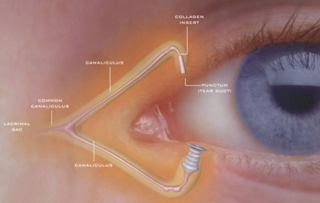

These plugs are made out of silicone or collagen and can be temporary, absorbable, or “semi-permanent”: meaning the stay in long term unless removed or pop out.
Some surgeons start patients on Restasis, Xiidra, and/or Autologous Serum right after LASIK if dryness is very bad.
Here is the link of all the dry eye treatments available to date:
https://drcremers.com/2018/05/step-ladder-2018-almost-all-treatments.html
Here is more information below.
SLC
Plasma Rich in Growth Factors for the Treatment of Dry Eye after LASIK Surgery.
Author information
- 1
- Fundación de Investigación Oftalmológica, Instituto Universitario Fernández-Vega, Oviedo, Spain.
- 2
- University Institute for Regenerative Medicine and Oral Implantology – UIRMI (UPV/EHU-Fundación Eduardo Anitua), Vitoria, Spain.
- 3
- Biotechnology Institute (BTI), Vitoria, Spain.
- 4
- Laboratory of Pharmacy and Pharmaceutical Technology, Faculty of Pharmacy, University of the Basque Country, Vitoria, Spain.
- 5
- Networking Biomedical Research Center on Bioengineering, Biomaterials and Nanomedicine, CIBER-BBN, SLFPB-EHU, Vitoria, Spain.
Abstract
PURPOSE:
MATERIAL AND METHODS:
RESULTS:
CONCLUSIONS:
Chronic dry eye symptoms after LASIK: parallels and lessons to be learned from other persistent post-operative pain disorders.
Author information
- 1
- Bascom Palmer Eye Institute, University of Miami, 900 NW 17th Street, Miami, FL, 33136, USA. alevitt@med.miami.edu.
- 2
- Bascom Palmer Eye Institute, University of Miami, 900 NW 17th Street, Miami, FL, 33136, USA. agalor@med.miami.edu.
- 3
- Miami Veterans Administration Medical Center, 1201 NW 16th St, Miami, FL, 33125, USA. agalor@med.miami.edu.
- 4
- Departments of Ophthalmology, Pathology and Pharmacology, Louisiana State University Health Sciences Center, Louisiana State University Eye Center, New Orleans, LA, USA. jweiss@lsuhsc.edu.
- 5
- Miami Veterans Administration Medical Center, 1201 NW 16th St, Miami, FL, 33125, USA. EFelix@med.miami.edu.
- 6
- Department of Physical Medicine and Rehabilitation, University of Miami Miller School of Medicine, Miami, FL, USA. EFelix@med.miami.edu.
- 7
- John P. Hussman Institute for Human Genomics, University of Miami Miller School of Medicine, Miami, FL, USA. EMartin1@med.miami.edu.
- 8
- John T Macdonald Foundation Department of Human Genetics, University of Miami Miller School of Medicine, Miami, FL, USA. EMartin1@med.miami.edu.
- 9
- Department of Anesthesiology, Perioperative Medicine and Pain Management, University of Miami Miller School of Medicine, Miami, FL, USA. dpatin@med.miami.edu.
- 10
- Department of Anesthesiology, Perioperative Medicine and Pain Management, University of Miami Miller School of Medicine, Miami, FL, USA. KSarantopoulos@med.miami.edu.
- 11
- Miami Veterans Administration Medical Center, 1201 NW 16th St, Miami, FL, 33125, USA. RLevitt@med.miami.edu.
- 12
- John P. Hussman Institute for Human Genomics, University of Miami Miller School of Medicine, Miami, FL, USA. RLevitt@med.miami.edu.
- 13
- John T Macdonald Foundation Department of Human Genetics, University of Miami Miller School of Medicine, Miami, FL, USA. RLevitt@med.miami.edu.
- 14
- Department of Anesthesiology, Perioperative Medicine and Pain Management, University of Miami Miller School of Medicine, Miami, FL, USA. RLevitt@med.miami.edu.


