&
How Best to Clean Your Eyelids:
The Controversy
For years, eyeMDs and optometrist have recommended cleaning the eyelids, also known as lid hygiene, as a way to keep bacteria and mites (now we know the latter to be a big issue for some patients) away from the eyelids and in particular the meibomian gland orifice. The hypothesis is that debris (ie, old cell, bacteria, mites, makeup) clog the meibomian gland orifice which then prevents the meibomian gland from pumping out its oil. This leads to a back up which can then lead to a stye (or sty) and eventually a chalazion in the eyelid: sometimes there are multiple ones of these. If not cleared quickly, this gland can scar permanently and never produce meibum (the precious oily part of the tear film) again.
How best to clean the eyelids is actually very controversial.
Some doctors recommend frequent lid cleaning, warm/hot compresses (without burning your skin) and eyelid massaging with attempts to express the oil from the eyelid margin.
Other doctors say things like the below by Dr. Brown: “Repeated expression can lead to the cells permanently adhering, causing obstructions deeper in the gland.”
The fact is that there is no randomized, controlled study to prove the later is true. I could not find any study supporting Dr. Brown’s statement: the full article is below. If you see a study to prove me wrong, please let me know. As far as I could see in the literature, we do not have molecular or even Lipiview proof to say that applying too much warm compresses is bad for your eyelids or leads to permanent damage. Clearly one should not apply so much heat as to chafe the skin
On the contrary, most MDs and ODs, including myself, feel the warmer the better, the longer the better, the more frequent massaging of the eyelids the better (in the form of blinking exercises and hard blinks after a warm/hot compress and gentle eyelid massages without feeling pain in the eyeball.)
This makes it very frustrating for patients that want a firm guideline on how to clean their eyelids.
Hopefully more studies like the ones below will begin to shed light on the following questions everyone has:
1. How hot should the compress be?
2. For how long should I put the compress on?
3. How exactly should I do the warm compresses?
4. How many times a day should I apply warm compresses?
5. Should I massage my eyelid margin?
6. How should I massage my eyelid margin?
7. Should I self-express my glands?
8. What drops should I use?
9. Is it ok to wear makeup?
10. Should I throw out my makeup?
11. How best should I dilute the Tea Tree Oil?
12. Is Avenova equivalent truly to Tea Tree Oil in getting rid of Demodex?
But there is some data to answer some of these questions:
1. How hot should the compress be?
Dr. Korb and Dr. Blackie, who are excellent optometrists, have done the most research on this question that I could find thus far:
Reported melting temperatures of normal meibomian secretions vary significantly with the majority of reports ranging from 32 to 40°C; severely obstructed meibomian glands have considerably higher melting points. Only using mildly warm water may not be adequate to relieve the meibomian gland obstruction. Therefore, each degree of temperature increase over 40°C could be critical in melting severely obstructed material. However, increasing temperature without safety controls raises the issue of potential thermal damage to the cornea [though I have never seen this or read a case report of burning the cornea as one would usually have so much pain from burning the skin that it would not be possible to burn the cornea with just a hot compress]. Based on the most conservative safety thresholds in the literature, temperatures below 40°C will not result in thermal injury to the cornea or crystalline lens.(Reference 1 below)
They created the LIPIFLOW machine which provides steady state temperature of 42.5°C for 12 minutes at the eyelid margin.
For daily cleaning, this means the water should be very warm but not hot enough to cause pain or burn the skin.
2. For how long should I put the compress on?
Dr. Korb says 15minutes is the best. But no one I know really has 15 minutes 2-3 times per day to do there warm compresses. Thus it may be better to do warm compresses more often (but not within 2 hours of each session–see below) 3 times a day instead of 2 times a day for as long as you can.
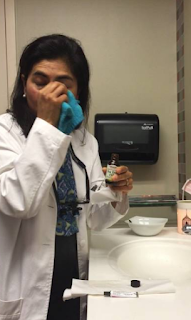
3. How exactly should I do the warm compresses?
The only good study I could find to say it was superior is called the Bundle Method.
Again, the bundle methods sounds lovely, but most patients I know do not have time to do this. Thus any type of dry or wet heat helps. How much it will help for you depends on many factors: how many glands you have, is there any scaring in the glands, your age, your hormone status, what other meds are you on.
4. How many times a day should I apply warm compresses?
Likely the best is at least 2-3 times per day.
What we do know is from a study by Dr. Korb & Dr. Blackie: the below tells us, you need to apply some pressure (not too hard) on the eyelids for about 8-20 seconds
“The results show that a single central meibomian gland can be drained of its liquid secretion in 8-20 seconds upon application of a constant force of 1 g/mm2. After a central optimally secreting gland has been drained of its liquid secretion, it takes a mean time of 2.17 ± 0.49 hours to again secrete liquid during waking hours, using the same amount of force to express the new liquid secretion. At that serial expression when liquid secretion is first observed, it then takes approximately half of the time required to drain the gland originally to redrain the gland, indicating a partial recovery. Furthermore, the minimal amount of liquid secretion obtained upon diagnostic reexpression after drainage suggests that a meibomian gland in this condition may contain inadequate liquid secretion to be available with habitual blinking, which applies a force less than 1 g/mm2.“ Reference 3,4 below.
5. Should I massage my eyelid margin?
Yes. Studies show massaging pumps out the oil, especially if the oil has been melted with warm compresses beforehand.
6. How should I massage my eyelid margin? And can I massage my eyelids too much?
This is a controversial one. I recommend massaging for 20 seconds with warm water applied to eyelids at same time (mostly to save time), or with a warm compress as noted below. The key thing to remember is that the warmer the better but do not burn your skin. I have not heard of massaging your eyelid too much if there are no skin issues.
7. Should I self-express my glands?
It depends on what we mean by “self-express.” Some patients I know pinch their eyelid margin trying to push out the oil for relief. I could not find any studies to show this is dangerous, but my main concern would be a potential corneal abrasion from scratching the eye. Using an instrument to self express again would be a concern for potentially scratching the cornea. As long as this self expression is not done too aggressively, it makes does not seem to be dangerous. But again we do not have good studies to show it is dangerous that I could find.
8. What drops should I use?
There are many that can be used. The best is a non-preserved tear. A ‘no-drug company money” study showed that Retaine is the best. I have a post on this which I will link up shortly.
9. Is it ok to wear makeup?
Likely yes as long as you are taking off the make up completely. I could not find any study saying make up permanently clogs the glands if removed. Many of my severe dry eye patients, though, have stopped being able to use make up as they do feel it makes their eyes feel worse even if they remove it completely.
10. Should I throw out my makeup?
When I was a resident, we used to recommend patients throw out their make up if we saw “Blepharitis”–the catch all phrase for bacteria and now Demodex mites seen on the microscope. We now know that the bacteria & mites will come back even if you get new make up. Likely it makes sense to throw out the make up every year or 2 but I do not have studies to back this up.
11. How best should I dilute the Tea Tree Oil?
Different patients and their skin prefer different dilutions. 50% dilution with coconut oil, mineral oil, olive oil is likely best. I use pure tea tree oil “diluted” on a warm wet towel to clean my eyes. Likely it does not dilute very much as oil and water do not mix, but this works best for me.
12. Is Avenova equivalent truly to Tea Tree Oil in getting rid of Demodex?
The Avenova company says they are but there are no head to head studies. I do use both and find both to work. I prefer Tea Tree Oil when my eyes feel particularly crusty or uncomfortable as one can feel it working. The Avenova feels like water but that is a good thing especially if you have very sensitive skin. My kids prefer Avenova!
1A.
All Warm Compresses Are Not Equally Efficacious.
Abstract
PURPOSE:
METHODS:
RESULTS:
CONCLUSIONS:
Meibomian gland therapeutic expression: quantifying the applied pressure and the limitation of resulting pain.
Abstract
OBJECTIVES:
METHODS:
RESULTS:
CONCLUSIONS:
Emerging strategies for the diagnosis and treatment of meibomian gland dysfunction: Proceedings of the OCEAN group meeting.
Author information
- 1Department of Ophthalmology, University Hospital Duesseldorf, Heinrich-Heine University, Duesseldorf, Germany. Electronic address: geerling@med.uni-duesseldorf.de.
- 2Centre Hospitalier National d’Ophtalmologie des Quinze-Vingts, University Paris-Saclay, Paris, France. Electronic address: chrbaudouin@aol.com.
- 3Institute of Ophthalmology, Department of Biomedical Sciences, University of Messina, Messina, Italy.
- 4Ocular Surface Centre, ISPRE Ophthalmics, Genoa, Italy.
- 5Department of Ophthalmology, Aristotle University of Thessaloniki, Thessaloniki, Greece.
- 6Hospital Clínico San Carlos, University Complutense, Madrid, Spain.
- 7Department of Ophthalmology, Bayındır Hospital, Ankara, Turkey.
- 8Instituto Universitario Fernández-Vega, University of Oviedo, Asturias, Spain.
- 9Service d’Ophtalmologie, CHU Bicêtre, APHP, Université Paris-Sud, Le Kremlin-Bicêtre, Paris, France.
- 10Department of Dermatology and UCD Charles Institute for Translational Dermatology, University College Dublin, Dublin, Ireland.
- 11Department of Ophthalmology, Ludwig Maximilian University, Munich, Germany.
Abstract
3.
https://dryeyeandmgd.com/i-wake-up-brush-my-teeth-and-clean-my-eyelids/
1. I WAKE UP, BRUSH MY TEETH AND CLEAN MY EYELIDS…
September 19, 2016

References:
———————————–
———————————–
———————————–
Although most diagrams of meibomian glands show a hollow tubular structure that looks like a permanently open space, a meibomian gland is more of a potential space. If the gland is empty of meibomian oils, it collapses in on itself. In fact even when the gland is “full” only a very thin film of oils may actually separate the cells lining the walls of the meibomian gland.
Meibomian oils are not squirted onto the surface of the eye. They seep out slowly under the gentle pumping action of eyelid blinking, combined with continuous oil production which pushes oils out onto the eye lid margin when the gland’s potential space is fully expanded.
When the eyelid margin becomes inflamed, this inflammation can “cap off” the meibomian gland orifices. There are numerous causes of eyelid margin inflammation that will not be discussed here. If the glands continue to vigorously produce oils, the oils erupt through the sides of the glands and coalesce into a mass commonly referred to as a stye. However in many patients, obstruction of normal oil seepage causes the meibomian gland to decrease production and the oils retained in the gland become thick and degraded.
In the past 2 – 4 years, eye care providers have become more widely aware of the connection between meibomian gland dysfunction and ocular surface symptoms. One simple office test is to lightly press on the glands while the patient is seated at the slit lamp. The examiner is looking for the quantity and quality of oils, how many glands express, how hard s/he has to push to make this happen, and how readily the oils disperse into the tear film. Meibomian oils are quite easy to see at the slit lamp but essentially impossible to see with the naked eye except through elaborate magnification methods.
Eye care providers sometimes prescribe meibomian gland self-expression or patients take it upon themselves to “clear out” their glands periodically. Generally the process is to apply heat to liquefy the oils, followed by eyelash cleaning (or sometimes the reverse order) and then gland expression.
First, not all meibomian gland problems are due to blockage of the orifices. If the glands are simply under-producing oils (a common problem in peri-menopausal women) pushing on them won’t do anything. If the lid margin inflammation is not under control and the orifices are tightly blocked, oils may not express even with hard pressure. So the treatment is not helpful. But secondly, self-expression can be harmful.
Remember that the gland is a potential space containing a small volume of oil. If you express all the oil out of the gland, you have probably expressed several days’ worth of “production”. You have depleted your supply. When the gland is empty, it collapses in on itself and the cells lining the potential space come into contact with each other without an intervening “oil slick”. This allows the cells to adhere to each other. As the gland refills with oil the potential space expands and the cells separate. Repeated expression can lead to the cells permanently adhering, causing obstructions deeper in the gland. This process will be hastened by the microtrauma induced through the mechanical pressure, especially if applied vigorously and often.
I have seen patients who have basically murdered their meibomian glands through excessive self-expression. How do I know? Because the glands in the far nasal and temporal (ear side) areas are harder to reach. It is also more difficult to apply direct firm pressure to the glands in the upper lids than to those in the lower lids. So I see more non-functioning glands in the centers of both lids than the corners, and the lower lids have more non-functioning glands than the upper lids.
When is self-expression helpful? Some patients have mildly occluded orifices or tend to produce oils that don’t seep well. They get into a “stagnation” situation. As part of their overall rehabilitation which MUST include efforts to improve oil quality and open the orifices, mild self-expression following a hot compress can be beneficial.
If you are a frequent (more than once per week) or aggressive self-expresser, ask yourself whether you are doing this “philosophically” because it seems like a smart thing to do or whether expressing truly improves your symptoms. If you are expressing several times per day, it is extraordinarily unlikely that you are getting a “useful” amount of oils onto the ocular surface each time. This habit will only increase the microtrauma to the meibomian gland structure.
Meibomian gland self-expression can be useful at certain stages of treatment. It is recommended by eye care providers, including those who specialize in ocular surface disease. It is important to understand that you can overdo it. You should not use self-expression unless instructed to do so by your eye care provider. If you have ocular surface pain and your provider has never expressed your glands, find a different doc.
What if you are a non-producer? Patients whose meibomian glands have ceased production are in a particularly difficult state. Peri- and post-menopausal women are most prone to this condition since meibomian gland function is regulated by androgen hormones. Some women become abruptly dry during pregnancy and don’t recover after pregnancy. Conversely some women have symptoms before pregnancy and actually feel better during pregnancy. We do not have a good understanding of the complex hormonal interplay that affects meibomian gland function. However, if your glands aren’t making oils because they aren’t receiving “go” signals from hormones or ocular surface nerves, many of the treatments described above will not be effective. Low production can combine with eyelid inflammation to further reduce the quality and quantity of oils reaching the tear film. Certainly related problems such as eyelid inflammation should be addressed. But for patients whose essential problem is markedly reduced production, it is particularly important to leave your meibomian glands alone!
heat – liquifies oils which tend to become more viscous just below body temperature (eyelid skin cooler than core body temp); see comments above about correct hot compress
doxycycline and minocycline, erythromycin – low dose for at least 60 days – acts as an anti-inflammatory which opens the orifices, thins out the oils in some fashion that we don’t understand, decreases the bacterial load on the eye lid margins which opens the orifices
TobraDex ointment – anti-inflammatory, decreased bacterial load; intraocular pressure must be followed if used for more than 1 month
Restasis – in my experience anti-inflammatory effects can improve meibomian gland inflammation as well
omega oils – antiinflammatory, antioxidant, ‘good ingredient’ for oil production
Azasite applied to eye lid margins (topical equivalent of erythromycin) – antibacterial, maybe something else as well? seems to work for some people not others