Punctal Plugs are generally very safe. Punctal Plugs got a bad wrap when one called the Smart Plug caused some issues with infections around the puncta and canal, called canaliculitis or dacrocystitis. That was around 2006.
The newer version of Punctal Plugs is much safer. I have never had a complication from the plugs we use.
More information about punctal plugs is located on my previous post:
https://drcremers.com/2018/01/which-is-best-punctal-plug.html
Management of complications after insertion of the SmartPlug punctal plug: a study of 28 patients.
Abstract
PURPOSE:
DESIGN:
PARTICIPANTS:
METHODS:
MAIN OUTCOME MEASURES:
RESULTS:
CONCLUSIONS:
Safety and Efficacy of Lacrimal Drainage
System Plugs for Dry Eye Syndrome
A Report by the American Academy of Ophthalmology
Marcus M. Marcet, MD,1 Roni M. Shtein, MD, MS,2 Elizabeth A. Bradley, MD,3
Sophie X. Deng, MD, PhD,4 Dale R. Meyer, MD,5 Jurij R. Bilyk, MD,6 Michael T. Yen, MD,7
W. Barry Lee, MD,8 Louise A. Mawn, MD9
Objective: To review the published literature assessing the efficacy and safety of lacrimal drainage system
plug insertion for dry eye in adults.
Methods: Literature searches of the PubMed and Cochrane Library databases were last conducted on
March 9, 2015, without date restrictions and were limited to English language abstracts. The searches retrieved
309 unique citations. The primary authors reviewed the titles and abstracts. Inclusion criteria specified reports
that provided original data on plugs for the treatment of dry eyes in at least 25 patients. Fifty-three studies of
potential relevance were assigned to full-text review. The 27 studies that met the inclusion criteria underwent data
abstraction by the panels. Abstracted data included study characteristics, patient characteristics, plug type,
insertion technique, treatment response, and safety information. All studies were observational and rated by a
methodologist as level II or III evidence.
Results: The plugs included punctal, intracanalicular, and dissolving types. Fifteen studies reported
metrics of improvement in dry eye symptoms, ocular-surface status, artificial tear use, contact lens comfort,
and tear break-up time. Twenty-five studies included safety data. Plug placement resulted in 50%
improvement of symptoms, improvement in ocular-surface health, reduction in artificial tear use, and
improved contact lens comfort in patients with dry eye. Serious complications from plugs were infrequent.
Plug loss was the most commonly reported problem with punctal plugs, occurring on average in 40% of
patients. Overall, among all plug types, approximately 9% of patients experienced epiphora and 10% required
removal because of irritation from the plugs. Canaliculitis was the most commonly reported problem
for intracanalicular plugs and occurred in approximately 8% of patients. Other complications were reported
in less than 4% of patients on average and included tearing, discomfort, pyogenic granuloma, and
dacryocystitis.
Conclusions: On the basis of level II and III evidence in these studies, plugs improve the signs and symptoms
of moderate dry eye that are not improved with topical lubrication, and they are well tolerated. There are no level I
studies that describe the efficacy or safety of lacrimal drainage system plugs. Ophthalmology 2015;122:1681-
1687 ª 2015 by the American Academy of Ophthalmology.
https://drcremers.com/2018/01/which-is-best-punctal-plug.html
Introduction
Dry eye is a common condition that occurs when the eye either does not have enough oil lubrication from the meibomian glands (called Meibomian Gland Dysfunction) and/or the eye’s lacrimal gland does not produce enough tears to keep the eye moist, comfortable, pain-free, and give crisp vision.
When relief from dry eye is not achieved by using warm compresses, cleaning with diluted Tea tree oil or Avenova spray (see video), increased oral Omega 3, artificial tears, or other lubricating products, Dr. Cremers often recommends punctal plugs of the eyelid’s puncta or permanent occlusion (if the plugs help but keep falling out).
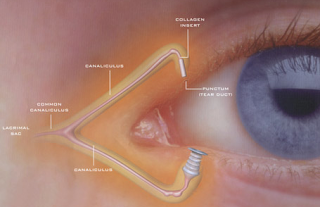
A Punctal plug is a tiny devices that occludes the 1 of the 4 puncta or drainage opening of the tear drainage system of the eye, so tears cannot drain into the nose. Punctal plugs are a non-drug procedure for dry eye when artificial tears do not sufficiently decrease dry eye symptoms (burning, redness, foreign body sensation, tearing, itching). This blockage tries to keep your natural tears in your eye longer and improve the quality and quantity of the tear film. One or all 4 openings can be covered or blocked at a time. Doctors often plug both lower eyelids first. If this is not enough, sometimes we will plug the upper puncta as well. If the lower 2 punctal plugs irriate the eye, we will take them out and plug the upper two puncta (or vice versa).
The most common side effects of occlusion are epiphora (overflow of tears), inhibited tear clearance, and desensitization of the corneal surface, or it does not help symptoms. Very rarely, the plug can lead to an infection in the area of the lacrimal sac or get stuck requiring surgical removal (I have not seen such a case occur but it has been reported).
Punctal Plugs can be classified according:
A. Location of placement:
1. Punctal (at surface of puncta opening)
2. Intracanalicular (deeper into punctal structure)
B. Duration of Placement:
1. Short Duration: Absorbable: made of animal collagen which absorb in about 4-14 days
2. Extended Duration/Semi-Permanent: do not absorb: usually stay in for 2-6 months but have seen them stay in for years.
C. Punctal plugs can be made out of:
 1. Silicone: which are semi-permanent; non-dissolving and may be removed in the future if desired or necessary.
2. Collagen: are temporary
1. Silicone: which are semi-permanent; non-dissolving and may be removed in the future if desired or necessary.
2. Collagen: are temporary
3. Other less commonly used materials:
a. hydrogel
b. polydioxanone
c. acrylic
D. 1 study from Egypt used Botox to cause punctal occlusion after LASIK but not usually done.
Collagen plugs generally dissolve within four to seven days, while silicone plugs either dislodge spontaneously or are removed by a technician, OD, or MD.
Surgeons typically prescribe the silicone punctal plugs first unless the patient really wants to try collagen plugs first as the collagen plugs dissolve in a few days (also there are more reports of complications with collagen plugs than silicone plugs as the silicone plugs have a little rim to generally prevent them from falling into the canal too deeply): see below report.
If the plugs keep falling out, thermal cautery or argon laser achieves permanent occlusion of the puncta.
Punctal Plugs can be classified according:
A. Location of placement:
1. Punctal (at surface of puncta opening)
2. Intracanalicular (deeper into punctal structure)
B. Duration of Placement:
1. Short Duration: Absorbable: made of animal collagen which absorb in about 4-14 days
2. Extended Duration/Semi-Permanent: do not absorb: usually stay in for 2-6 months but have seen them stay in for years.
 1. Silicone: which are semi-permanent; non-dissolving and may be removed in the future if desired or necessary.
1. Silicone: which are semi-permanent; non-dissolving and may be removed in the future if desired or necessary.3. Other less commonly used materials:
a. hydrogel
b. polydioxanone
c. acrylic
- Electrodesiccation – closing off with electricity
- Thermal cautery – closing off with heat
- Argon Laser– closing off with Laser: not covered by insurance
- Argon Laser– closing off with Laser: not covered by insurance
Very occasionally, permanent occlusion may need to be repeated in order to be fully effective. If a patient wants to “undo” the permanent closure, it may require a plastic surgeon to reopen the puncta and canal.
There are NO randomized controlled studies to prove one punctal plug is better than the other. Also, given the complexity of the dry eye syndrome and disease, there are no good studies to conclusively prove punctal plugs improve dry eye symptoms for every patient or for even the majority of patients. Still, this procedure is worth a try as it is very low risk and does help patients with their dryness. It may not work for you, but it is worth a try in most patients. It can help prevent the need for using steroid drops for dryness which has the risk of cataract requiring surgery and glaucoma (which is a potentially blinding disease) and is covered by most insurances.
More Information about These Procedures and Permanent Occlusion:
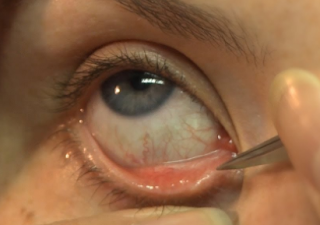
Plug insertion is performed in an examination room; it does not require a surgery center. Once you have been checked in and settled comfortably, drops will be used to numb your eye; no injections are needed.
We will ask you to look up and away from your nose. If plugs are being inserted, a forceps-like applicator will be used to place one into the corner of your eye to insert the plug into the orifice of the punctal canal. The entire procedure takes only a few minutes.
The procedure is basically the same for permanent occlusion, only a small injection of anesthesia is given to numb the area. A device is used to seal off (cauterize) the opening and nothing is inserted.
Many patients report immediate relief from dry eye symptoms and resume normal activities immediately. Serious complications with punctal occlusion are extremely rare, but like any medical procedure, it does have some risks. If you experience any discomfort with the semi-permanent plugs, Dr. Cremers can easily remove them.
Here is more information about Systemic Reviews of all the data on Punctal Plugs.
Sandra Lora Cremers, MD, FACS
1.
Ophthal Plast Reconstr Surg. 2009 Sep-Oct;25(5):413-4. doi: 10.1097/IOP.0b013e3181b57c01.
We will ask you to look up and away from your nose. If plugs are being inserted, a forceps-like applicator will be used to place one into the corner of your eye to insert the plug into the orifice of the punctal canal. The entire procedure takes only a few minutes.
The procedure is basically the same for permanent occlusion, only a small injection of anesthesia is given to numb the area. A device is used to seal off (cauterize) the opening and nothing is inserted.
Here is more information about Systemic Reviews of all the data on Punctal Plugs.
Sandra Lora Cremers, MD, FACS
1.
Canaliculitis with a papilloma-like mass caused by a temporary punctal plug.
Author information
Abstract
Absorbable plugs are used before attempting permanent occlusion to observe whether the patient will be amenable to treatment for dry eye. Little is known about the complications of absorbable plugs. The authors present a case of canaliculitis with a papilloma-like mass caused by long-standing unabsorbed collagen plug that had been placed 3 years earlier. This is an uncommon clinical presentation that may be encountered in patients who have canaliculitis symptoms and a history of intracanalicular temporary plug placement.
Main results
References:
(Balaram 2001; Freeman 1975; Willis 1987)
(AAO 2003; Dohlman 1978; Lemp 1994).
(Barnard 1996; Dohlman 1978; Tai 2002).