Scleral Lenses have been used for years to treat patients with chronic eye pain and/or chronic dry eye.
Doctors and surgeons often see that some patients do really well with Scleral Lenses while others really cannot tolerate them. Why is there this difference?
It likely relates to many factors:
1. What is the Schirmer’s test results: how much aqueous is produced?
2. Are the puncta of the 4 lids wide open or close: does the tear stay in cul de sac longer or does it clear into the nose too quickly?
3. Is Lid Wiper Epitheliopathy present: does constant blinking irritate the cornea nerves?
4. What do the meibomian glands look like and are they releasing enough meibum (ie, lipid/fat) into the tear film to prevent evaporation?
5. How much time is a patient on an electronic screen and what is the quality of the blink? Do they have incomplete blinks
6. Do they have an autoimmune disease?
7. Did they take Accutane: which likely affects the Lacrimal Gland, the Meiboomian Gland, and likely even the Goblet cells.
These are the key factors that can affect one’s acceptance of Scleral Contact Lenses.
A dear patient presented another issue which I have not heard about before:
“I believe the difference is due to the glycocalyx and goblet cell count (and probably also Lubricin production). Both are essential for lubricity in the eye.
The glycocalyx is destroyed or dramatically decreased due to long-standing inflammation. The average Sjogren’s patient has no glycocalyx at all!
The glycocalyx is especially vital for boundary lubrication during the blink (where the lid moves from a stationary position into motion)
I think a viable strategy is to double up on anti-inflammatories (Cyclosporine [Restasis or Cequa]and lifitegrast [Xiidra] both 4x daily) for a few months to improve ocular surface lubricity before maintaining eye health with sclerals. I’ve been trying that as of 4 days ago. I’ll let you know how it goes. Previously I couldn’t tolerate sclerals due to very high friction.
https://www.europeanreview.org
This paper is an analysis of factors leading to lid wiper epitheliopathy and shows that friction is mainly the result of low goblet cell count. Goblet cells are destroyed by the inflammatory cytokine IFN-y.”
Thus if a patient has a poor glycocalyx level, Scleral Contact Lenses likely will not provide the comfort one needs.
It’s a great question. It’s not really possible to clinically right now. However, if a patient with a decent tear meniscus (like mine with 4 plugs) is experiencing severe friction and lid wiper epitheliopathy in sclerals then the evidence suggests goblet cell:glycocalyx depletion is why. Both due to long standing inflammation. It’s possible that a patient would be able to tolerate again after an extended period of anti inflammatory therapy
I’m testing this on myself. Many unanswered questions: will it work, and if it does, can the effect be maintained by continuing Scleral use and winding down xiidra and cyclosporine use?
Lubricin is present in the joints and the eye and dramatically reduces friction in both. Likewise in both joints and the eye it’s production is seriously hampered by the presence of inflammatory cytokines
A synthetic version called lubris will be commercially available in the next few years
What Are Scleral Contact Lenses?
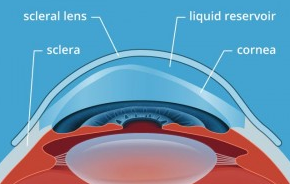
Scleral contacts are gas permeable contact lenses with a larger than normal diameter designed to vault and sit on the sclera (or white part of the eye) to prevent the eyelid from rubbing on the sensitive corneal nerves and/or to give an irregular cornea a smoother surface.
By preventing the rubbing of the upper lid on the cornea, conditions such as Lid Wiper Epitheliopathy can be limited.
By providing a smoother surface, the Scleral Lens can correct the vision issues caused by keratoconus or other irregularities.
Scleral Lenses can also function to hold extra fluid, such as a patient’s own tears, which can help patients with eye pain and chronic dry eye. (Some have place autologous serum or Platelet Rich Plasma under the Scleral Lens for short periods of time: there is a risk of corneal infection if done for long periods of time though the literature on the amount of time or even this practice is limited; there are some reports of corneal infection with Scleral Lens with and without the use of Serum or PRP).
Types of Scleral Contact Lenses
While larger than the standard contact lens, the scleral contact lens is still gas permeable. The sizes of these lenses can range from 14.5mm to 24mm. Anything below 18mm is considered a mini Scleral Contact Lenses. A Scleral Contact Lenses usually covers the entire cornea & limbus as the average cornea has an 11.8mm diameter. A normal contact lens (not Scleral) only covers around 80% of the cornea.
Sizes vary. Smaller Scleral Contact Lenses can be used in patients with mild Keratoconus. Smaller scleral lens are easier to apply, require less care and can cost less. Sometimes larger Scleral Contact Lenses are needed for patients with advanced Keratoconus or severe dry eye patients/chronic eye.
Scleral Contacts Lenses: Often Used to Treat Keratoconus but Can be used for Chronic Eye Pain, Chronic Dry Eye Discomfort, Chronic Foreign Body Sensation
Switching to a large-diameter Scleral Contact Lenses may help patients with Keratoconus or Lid Wiper Epitheliopathy/Dry eye disease/Meibomian gland dysfunction. Having a contact lens that rests on the less sensitive surface of the sclera can give relief and comfort to someone with keratinous. The scleral lens is designed to fit with minimum movement during blinks, which makes for a more stable and comfortable lens. Scleral contact lenses not only help those with Keratoconus but also those with other eye problems as well. If you suffer from severe dry eyes, have undergone a cornea transplant or even have Sjogren’s syndrome, scleral contact lenses may work for you.
Risks of Scleral Contact Lenses:
Cost of Scleral Contact Lens
Scleral lens are custom made for each user which means they are going to be more expensive than the standard contact lens. Many vision insurance programs fully cover scleral contact lens fittings and can cut the cost of your lens. Contact us if interested: 301-896-0890 or text 240-706-0313.
References:
https://content.iospress.com/articles/clinical-hemorheology-and-microcirculation/ch179235
https://emedicine.medscape.com/article/1192919-overview#a5
Normal conjunctival epithelial cells contribute to tear film stability through secretion of tear mucins, promotion of tear adherence to the glycocalyx, and provision of increased surface area for tear adherence via the microvilli. A transmission electron microscopy study by Koufakis et al evaluating conjunctival surface changes in patients with Sjögren syndrome demonstrated significant alterations of the apical conjunctival epithelium. [19] The study found a decreased number of microvilli per epithelial length, decreased microvillus height and height-width ratio, and a decreased number of secretory vesicles per epithelial cell in patients with Sjögren syndrome as compared with controls. [19] Furthermore, the ocular surface glycocalyx (OSG) in patients with Sjögren syndrome was either not detectable (in most cases) or severely altered in configuration compared with the OSG of healthy controls.