by Sandra Lora Cremers, MD, FACS
They are designed to treat myopia (nearsightedness), hyperopia(farsightedness) and astigmatism, and can allow you to live without glasses or contacts in most cases.
Sight-threatening complications, such as significant loss of vision or infection from LASIK, PRK, etc surgery are thankfully extremely rare, and many side effects, such as residual (left over) astigmatism or refractive error and laser eye surgery complications (such as folds, inflammation, flap dislocation, small infections, which are rare) can be resolved with additional surgery or medical treatment.
First, choose a skilled, experienced, ethical LASIK/PRK eye surgeon can help reduce these risks and enable you to achieve the best possible results from laser eye surgery. I have seen too many patients have LASIK when they should not have had it performed on their eye.
Questions to Ask Your Surgeon:
by Sandra Lora Cremers, MD, FACS
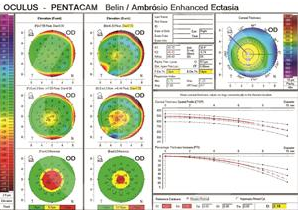 if this little box on right of photo is red, you should not have LASIK/PRK. If it is yellow, you are at risk of developing ectasia after LASIK/PRK. The risk depends on how thin your cornea is in relation to the amount of refractive error (your glasses RX) the surgeon thinks should be treated.
if this little box on right of photo is red, you should not have LASIK/PRK. If it is yellow, you are at risk of developing ectasia after LASIK/PRK. The risk depends on how thin your cornea is in relation to the amount of refractive error (your glasses RX) the surgeon thinks should be treated. 13. This one is not a question you need to determine on your own, but you can ask your surgeon: Is your (the patient) personality the type of personalities that do well after LASIK. Many surgeons know that a type AAA++ personality will notice every imperfection and will not be satisfied unless everything is perfect. Many have noted that doing LASIK on engineers, lawyers, physicists, is generally a higher risk procedure because they will notice everything. It is not a contraindication, but know many times everything is not perfect, and some people have to live with slight, noticebale imperfections in their vision and/or in how their eye feels. If you cannot imagine such a possiblity, do not have LASIK/PRK.
LASIK Eye Surgery Risk Factors And Limitations
- Too thin or irregular corneas
- Large pupils
- High refractive error
- Unstable vision: changing Rx
- Dry eyes: gritty eyes?
- Your age
- If you are pregnant
- If you have certain degenerative or active autoimmune disorders
| Complications | Symptoms | Treatments |
|---|---|---|
| Incomplete corrections (undercorrection, overcorrection, residual astigmatism) or regression of effect | Poor quality vision; Blurry, less-than-perfect vision | Glasses or contact lenses; eye drops; re-treatment with laser |
| Decentered ablations | Visual aberrations* | Eye drops; re-treatment with laser |
| Oversize pupils | Visual aberrations* | Eye drops; re-treatment with laser |
| Haze | Visual aberrations* | Eye drops; re-treatment with laser |
| Irregular flap (folds, wrinkles, striae) | Visual aberrations* | Surgical correction; second laser procedure |
| Dry eye | Dry, itchy or scratchy eyes, often with redness and sense of foreign object in eye, and sometimes pain | Warm Compresses (see below video); Prescription dry eye medication; artificial tears; Xiidra, Restasis, punctal occlusion (blockage of tear ducts in order to retain tear film on eye), Omega 3, autologous serum, LipiFlow, IPL, Meibomian Gland Probing; Steroid drops |
| Diffuse lamellar keratitis (eye inflammation) | Visual aberrations* | Eye drops; surgical rinsing of cells if severe |
| Epithelial ingrowth | Visual aberrations* | Surgical removal of epithelium |
| Infection | Discharge, Redness, oozing of eyes, sometimes pain | Eye drops; oral medications |
| *Visual aberrations include symptoms such as glare, double vision, ghosting, halos, starbursts, loss of contrast sensitivity, and problems with low-light or night vision. Most patients do not experience these symptoms, and some patients with these complications experience no symptoms and require no treatment. | ||
How Common Are LASIK Complications?
HOW TO SAVE YOUR MEIBOMIAN GLANDS
What is SPK? Superficial Punctate Keratitis
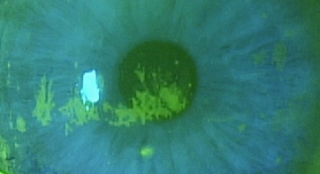
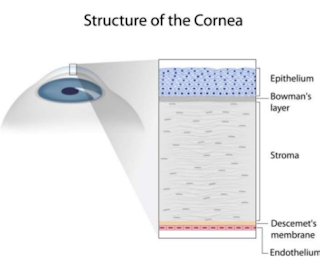
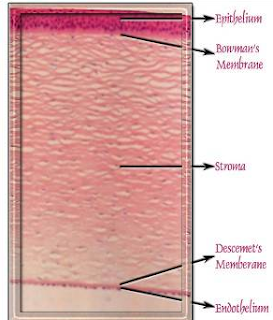
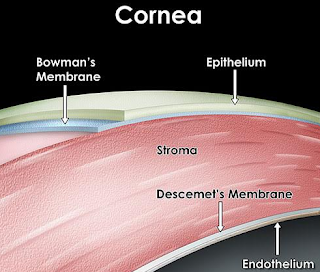
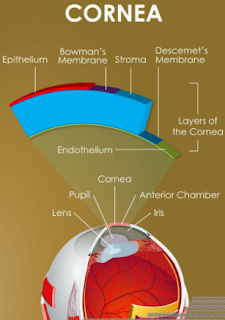 Superficial Punctate Keratitis means that the surface of the Cornea is so dry from Inflammation (-itis…thus keratitis: -kera means Cornea), that the Cornea’s surface epithelial cells have died and left a bare area of underlying Bowman’s membrane (the layer under the epithelium). When we put a yellow drop called Fluoresceine, it stains Bowman membrane cells and not healthy epithelial cells. This is how we can see under the microscope that a patient has dry eyes.
Superficial Punctate Keratitis means that the surface of the Cornea is so dry from Inflammation (-itis…thus keratitis: -kera means Cornea), that the Cornea’s surface epithelial cells have died and left a bare area of underlying Bowman’s membrane (the layer under the epithelium). When we put a yellow drop called Fluoresceine, it stains Bowman membrane cells and not healthy epithelial cells. This is how we can see under the microscope that a patient has dry eyes.
Why do Corneal Epithelial Cells Die?
Corneal Epithelial Cells die from:
1. Direct trauma, like a scratch on your eye or corneal abrasion.
2. Chemicals: getting an acid or base will kill these cells and many other important eye surface cells.
3. LASIK and PRK: we cut the cornea in LASIK or remove the epithelial cells in PRK, and thus purposely remove these cells to sculpt the shape of the cornea to help get a patient glasses free. The risk of doing this is that in some patients, especially if they have decreased Meibomian Glands and/or Dry Eye, the epithelial cells and maybe even the corneal nerves, do not grow back “normally” and the patient feels dry eyes that does not go away.
4. Dry Eye: this is a big issue. Dry Eye can be caused by many things, genetics, aging, hormonal changes, chronic computer use (see below), Meibomian Gland Dysfunction
5. Meibomian Gland Dysfunction: I think a patient can hit a tipping point where the extent of Meibomian Gland loss and oil production loss is significant enough to directly kill corneal epithelial cells. Likely with decreased meibomian glands and oil production, the corneal epithelial cells hit a point chemically where they behave as if to say “I can’t take this milieu/environment any more: I guess I will just disappear.” This then shows us SPK.
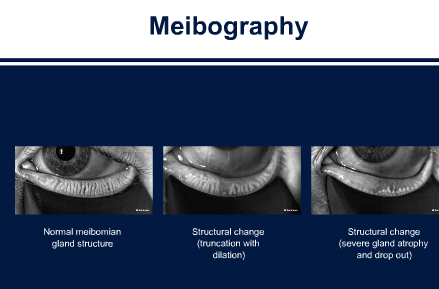
We can now image Meibomian Glands clearly for the first time ever. I would venture to say that a patient should not have LASIK or PRK unless they see for themselves their Meibomian Glands on LipiView or LipiScan. This will give them a better idea of what the risk is of having chronic dry eye, chronic halos/glare, chronic discomfort/foreign body sensation, chronic decreased quality of vision even with 20/20 vision which is a real complaint in LASIK and PRK patients.
If the meibomian glands loss is severe, I do not think that patient should have LASIK or PRK. The risk is too great of chronic debilitating eye discomfort, pain, and vision loss.
Normal Meibomian Glands should look like “White Piano Keyes Filled with Oil” On Meibography or LipiScan or LipiView Machines seen on bottom left.
Aging, genetics, chronic blepharitis and meibomian gland dysfunction, poor diet, smoking, inflammatory issues and disease, radiation, chemotherapy, previous surgery, and I must add Chronic computer/video game/cell phone use (ie, Computer Vision Syndrome or a new term I will coin called Decreased Blinking Quality Syndrome or Decreased Blinking Rate Syndrome which can happen to even avid readers, skiers, etc) can destroy these precious glands and cause them to never function again. This loss of meibomian glands, decreases the ability of the tears to lubricate the cornea properly, which then leads to the death of the corneal epithelium, thus giving SPK. The death of the corneal epithelium, though is reversible.
To date, I have had 5 patients whose Meibomian Glands showed “growth” or improvement after LipiFlow or Intense Pulse Light or Meibomian Gland Probing. The current thought, though is that once a meibomian gland is gone, it is gone for good. I hope I am right.
On the right you can see:
Severe Meibomian Gland Loss
References:
Refractive surgeries, such as laser in situ keratomileusis (LASIK) and laser-assisted subepithelial keratomileusis (LASEK), have been popularized for correction of low to moderate myopia.6 ; 7 Vision-threatening posterior segment complications can occur after refractive surgeries; they include macular hemorrhages, macular holes, and rhegmatogenous RD.8; 9; 10; 11; 12; 13 ; 14 The reported incidence of rhegmatogenous RD in those with histories of LASIK is not high, ranging from 0.033% to 0.25%.11; 15; 16 ; 17However, many have regarded a suction ring application during LASIK to be a potential risk factor for rhegmatogenous RD because this procedure may induce vitreous traction and detachment resulting from sudden decompression of the eye.18 ; 19 A previous study found that retinal breaks were more commonly located in the inferotemporal quadrant in rhegmatogenous RD after LASIK.20 Whether this feature is characteristic of rhegmatogenous RD after LASIK is unclear because this finding was not compared to rhegmatogenous RD without prior LASIK.
-
-
6-
A corneal flap technique for laser in situ keratomileusis. Human studies
-
Arch Ophthalmol, 109 (12) (1991), pp. 1699–1702
-
|
|
-
- 7
-
Laser in situ keratomileusis for myopia from −5.50 to −11.50 diopters with astigmatism
-
J Refract Surg, 14 (1) (1998), pp. 19–25
-
|
-
- 8
-
Posterior segment complications after laser-assisted in situ keratomileusis
-
Curr Opin Ophthalmol, 19 (3) (2008), pp. 177–184
-
|
|
-
- 9
-
Bilateral retinal detachment associated with giant retinal tear after laser-assisted in situ keratomileusis
-
Retina, 18 (2) (1998), pp. 176–177
-
|
|
-
- 10
-
Retinal detachment in myopic eyes after laser in situ keratomileusis
-
Am J Ophthalmol, 128 (5) (1999), pp. 588–594
-
|
|
|
-
- 11
-
Rhegmatogenous retinal detachment after laser-assisted in situ keratomileusis (LASIK) for the correction of myopia
-
Retina, 20 (4) (2000), pp. 338–341
-
|
|
-
- 12
-
Retinal detachment associated with excimer laser
-
Curr Opin Ophthalmol, 10 (3) (1999), pp. 173–176
-
|
|
-
- 13
-
Bilateral macular hemorrhage after laser in situ keratomileusis
-
Graefes Arch Clin Exp Ophthalmol, 237 (7) (1999), pp. 611–613
-
|
|
-
- 14
-
Full-thickness macular hole after LASIK for the correction of myopia
-
Ophthalmology, 112 (7) (2005), pp. 1207–1212
-
|
|
|
-
- 15
-
Incidence of vitreo-retinal pathologic conditions 24 months after laser-assisted in situ keratomileusis (LASIK)
-
Ophthalmology, 107 (2) (2000), pp. 258–262
-
|
|
|
-
- 16
-
Retinal detachment after laser in situ keratomileusis in myopic eyes
-
Am J Ophthalmol, 144 (6) (2007), pp. 921–923
-
- 17
-
Retinal detachment following laser in situ keratomileusis
-
Ophthalmic Surg Lasers, 31 (2) (2000), pp. 121–125
-
|
-
- 18
-
Rhegmatogenous retinal detachment in myopic eyes after laser in situ keratomileusis: frequency, characteristics, and mechanism
-
J Cataract Refract Surg, 27 (5) (2001), pp. 674–680
-
|
|
|
-
- 19
-
Proposed mechanism for retinal tears after LASIK: an experimental model
-
Ophthalmology, 111 (1) (2004), pp. 24–27
-
|
|
|
-
- 20
-
Rhegmatogenous retinal detachment after LASIK for myopia of up to −10 diopters: 10 years of follow-up
-
Graefes Arch Clin Exp Ophthalmol, 250 (7) (2012), pp. 963–970
-
-